Anesthesiology Residency Interview Questions Guide
Are you preparing for your Anesthesiology residency interview? This guide distills what makes Anesthesiology unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Anesthesiology residency interview.
Table of contents
What Makes Anesthesiology Unique
| Patient population | Anesthesiologists care for a vast and diverse patient population, spanning all ages from newborns to the elderly, encompassing anyone undergoing surgery or requiring sedation. This includes healthy individuals for routine cases, as well as critically ill or trauma patients. The specialty's breadth extends across subspecialties like pediatric, obstetric, cardiac, neuro, pain, and critical care anesthesia, demanding tailored care for each unique patient. |
| Approaches to care | Anesthesiologists blend deep knowledge of pharmacology and physiology with hands-on procedural skills. Their approach involves thorough preoperative assessment, selecting appropriate anesthetic techniques (general, regional, or sedation), and meticulously preparing contingency plans ("Plan A, B, C") for critical aspects like airway and hemodynamics. Intraoperatively, they continuously titrate drugs and fluids to maintain patient stability, and postoperatively, they ensure safe pain control and smooth transitions of care, increasingly utilizing advanced tools like point-of-care ultrasound. |
| Ethical dilemmas | Ethical dilemmas in Anesthesiology often arise from patients' extreme vulnerability, as they are typically unconscious and unable to advocate for themselves. Key challenges include obtaining informed consent for procedures where the patient will be unconscious, navigating advance directives (like DNRs) in the operating room, and balancing the imperative to "do no harm" with the need for intervention, such as ensuring adequate pain relief without over-sedation. Anesthesiologists uniquely serve as patient advocates when patients cannot speak for themselves, making communication and patient-centered decision-making paramount. |
| Current trends & controversies | Anesthesiology is rapidly evolving with significant trends in workforce and practice models, including new team-based care and efficiency initiatives driven by increasing demand and a looming shortage. Non-OR anesthesia (NORA) is a growing area presenting new safety challenges. Pain management is a hot topic, with anesthesiologists leading "opioid-sparing" care through multimodal analgesia and regional blocks to mitigate addiction risks. Technology and research trends involve leveraging simulation and artificial intelligence for safety improvements (e.g., AI decision-support for drug dosing) and exploring pharmacogenomics, blending acute physiology management, patient advocacy, and cutting-edge technology. |
Distinctive Aspects of Anesthesiology
1. Comprehensive Perioperative Physiology Management
Anesthesiologists oversee patients from pre-op through recovery, with constant vigilance on airway, breathing, and circulation. They must anticipate and respond to rapid physiological changes, always preparing multiple backup plans. This "plan A, B, and C" mindset and focus on life-support is unique to anesthesia.
2. Patient Vulnerability and Advocacy
Patients undergoing anesthesia are unconscious and helpless. Anesthesiologists must quickly build trust during brief pre-op encounters, communicate clearly about risks and options, and act as advocates in the OR. They often make critical decisions without the patient's direct input (e.g. interpreting advance directives or intraoperative preferences).
3. Pain Management Expertise
Pain control is a core competency of anesthesiology. Specialists in anesthesia also often sub-specialize in pain medicine, treating acute, chronic, and cancer pain. Candidates must appreciate multimodal analgesia techniques (nerve blocks, epidurals, non-opioid drugs) and the perioperative opioid stewardship role of the specialty.
4. Diverse Clinical Contexts and Settings
Anesthesiologists work in a wide range of settings beyond the hospital OR -- including ambulatory surgery centers, ICUs, labor and delivery suites, and radiology/endoscopy units (NORA). Each context has unique protocols and patient considerations (e.g. sedation techniques for MRI vs anesthesia for open surgery). The specialty's breadth across subspecialties (pediatric, obstetric, cardiac, neuro, etc.) also demands adaptability.
5. Technology, Safety Culture, and Trends
Anesthesiology is highly technology-driven, with advanced monitors, simulation training, and emerging AI tools shaping practice. Patient safety (e.g. safety checklists, electronic records) is paramount. Trainees must be aware of evolving controversies (e.g. CRNA vs MD roles, outpatient anesthesia models) and innovations like enhanced recovery protocols and AI support systems that are specific to this field.
Anesthesiology Residency Interview Questions & How to Answer Them
Preparing for your Anesthesiology residency interview means demonstrating not only your clinical knowledge but also your critical thinking, ethical reasoning, and commitment to patient safety and advocacy. Here are some common questions you can expect, along with guidance on how to craft exceptional answers.
1) How would you explain the risks of anesthesia to a patient in a way they can understand and feel reassured?
What the interviewers are looking for: This question assesses the candidate’s communication skills, empathy, and ability to build trust and provide reassurance in a high-stakes, emotionally charged situation. Anesthesiologists often have only a brief pre-operative encounter to explain complex medical information (risks of anesthesia) to anxious patients and their families. The interviewer wants to know if the candidate can translate medical jargon into understandable language, manage patient fear, and ensure informed consent while maintaining a compassionate and patient-centered approach. Essentially, it gauges the applicant’s emotional intelligence and their understanding of the anesthesiologist's role as a patient advocate, especially when the patient is at their most vulnerable.
How to excel in your answer
- Create a calm, private space and make eye contact right away.
- Start by acknowledging their nervousness and showing empathy.
- Use simple words and analogies (like 'pilot for surgery') to explain anesthesia and your role.
- Be honest about risks, but clearly separate common, mild side effects from very rare, serious ones.
- Highlight all the safety measures, constant monitoring, and your dedicated team to reassure them.
- Ask questions, pause for them to process, and use the 'teach-back' method to ensure they understand.
Mistakes to avoid:
- Don't use too much medical jargon or dismiss their fears with phrases like 'don't worry'.
- Avoid rushing or making it seem like you're just trying to get through a checklist.
- Don't make it all about you; focus on the patient's perspective and comfort.
- Don't just list risks without explaining why serious ones are rare and what precautions you take.
2) How do you prepare an anesthesia plan for a high-risk surgical patient?
What the interviewers are looking for: They want to see if you can think critically, plan ahead, and keep high-risk patients super safe during surgery. It's about showing you understand the anesthesiologist's role as a patient's advocate before, during, and after the operation.
How to excel in your answer
- Start by doing a deep dive into the patient's medical history, physical exam, and all their tests to really understand their risks.
- Explain how you'd try to get the patient in the best shape before surgery, even if it means calling other specialists.
- Show you're always thinking ahead! Mention having backup plans (like Plan A, B, C) for critical things like airway issues or sudden vital sign changes.
- Talk about how you'd pick the right anesthesia technique and what advanced monitors you'd use to keep a super close eye on them.
- Don't forget clear communication with the whole surgical team and how you'd make sure the patient's wishes are respected, especially since they can't speak for themselves.
Mistakes to avoid:
- Don't give a super simple answer like 'just be careful.' They want to hear your detailed, systematic approach!
- Avoid sounding reactive ('I'll deal with problems when they happen'). Show you're proactive with backup plans.
- Don't focus only on one thing (like just drugs) and ignore the big picture of patient assessment, optimization, and recovery.
- Don't forget to mention coordinating with the entire surgical team and other healthcare providers.
3) How would you respond if a patient under anesthesia developed a sudden life-threatening complication?
What the interviewers are looking for: This question checks if you can think fast, act decisively, and keep a cool head when a patient under anesthesia suddenly gets really sick. They want to see if you know how to keep patients safe when they're most vulnerable.
How to excel in your answer
- Immediately call for help from your attending and the surgical team while starting actions.
- Quickly check the patient's ABCs (Airway, Breathing, Circulation) and all monitors.
- Rapidly consider possible causes and start immediate, specific treatments.
- Communicate clearly and calmly with everyone in the room (surgeon, nurses, etc.), delegating tasks.
- Stay composed, lead the response, and show confidence in your training to stabilize the patient.
Mistakes to avoid:
- Don't panic or freeze; show you can act decisively.
- Avoid just waiting for your attending to tell you what to do; take initiative while calling for help.
- Don't sound passive or lack confidence in your ability to start interventions.
Other residency interview questions for Anesthesiology you should rehearse
- How do you handle disagreements with a surgeon regarding anesthetic management during a case?
- What would you do if a patient refuses anesthesia or a blood product needed for safe surgery?
- How would you handle a situation where a patient’s advance directive conflicts with the needs of surgery?
- How would you respond if a patient refused a blood product that you believed was necessary for safe care?
- How would you design a perioperative pain plan that minimizes opioid use while still providing effective pain control?
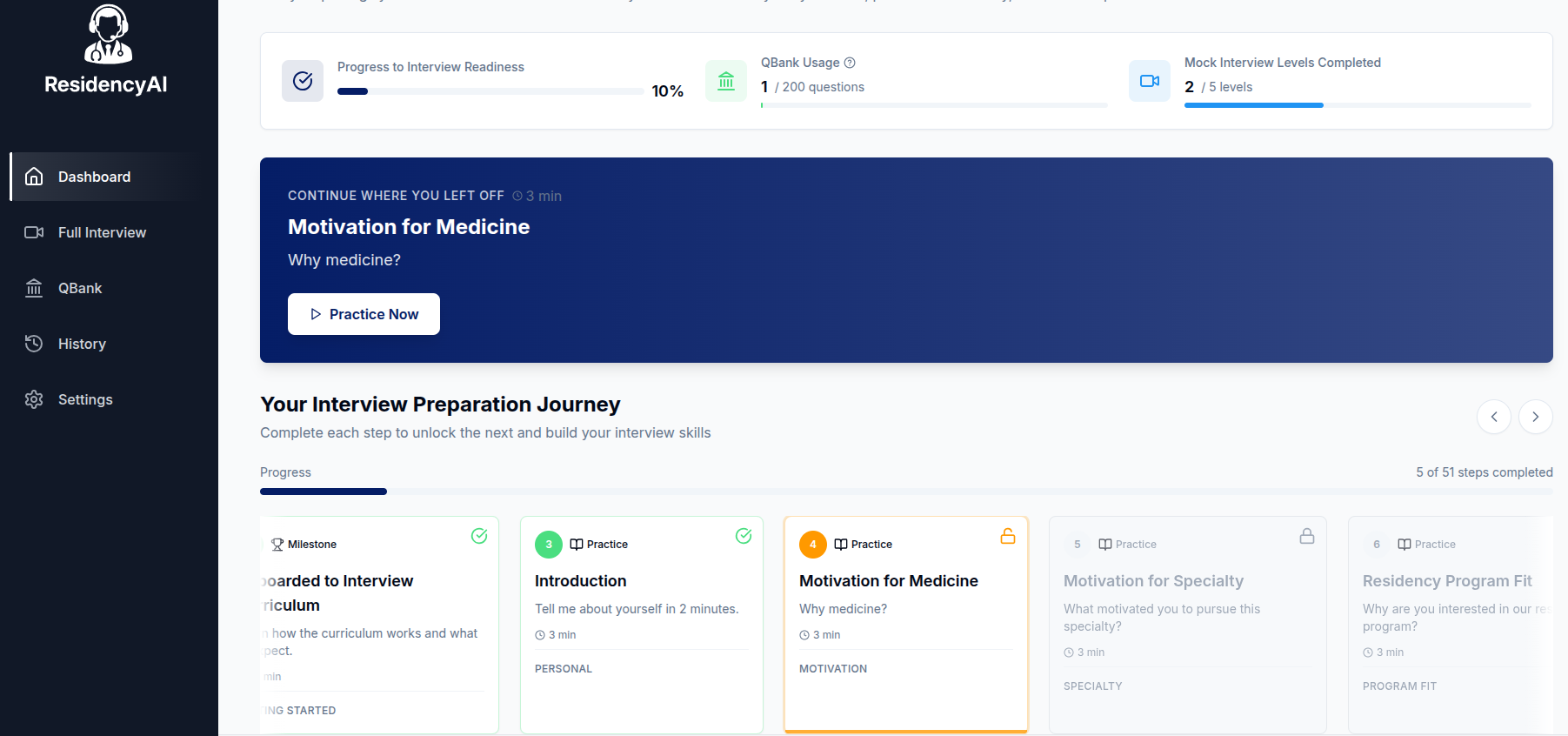
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.