Emergency Medicine Residency Interview Questions Guide
Are you preparing for your Emergency Medicine residency interview? This guide distills what makes Emergency Medicine unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Emergency Medicine residency interview.
Table of contents
What Makes Emergency Medicine Unique
| Patient population | Emergency Medicine (EM) physicians encounter an exceptionally broad and diverse patient population, encompassing all ages (from neonates to centenarians) and acuity levels, from healthy athletes to chronically ill elders, and from injured children to psychiatric emergencies. The Emergency Department often functions as a crucial healthcare 'safety net,' providing care for uninsured, homeless, or otherwise vulnerable patients who may lack other access to medical services. EM doctors must be prepared to treat 'everything from earaches to Ebola' across various communities. |
| Approaches to care | EM physicians manage a vast spectrum of clinical problems, from minor complaints like superficial injuries and respiratory infections to life-threatening crises such as trauma, acute cardiac events, and neurologic emergencies. A defining aspect of EM is the management of undifferentiated patients (e.g., altered mental status or shock of unknown cause), requiring rapid hypothesis-generation and a broad diagnostic workup. The core approach emphasizes rapid assessment and stabilization of life-threatening conditions, utilizing established protocols (like ACLS for cardiac arrest and ATLS for trauma) and point-of-care tools (such as bedside ultrasound) for immediate diagnosis. EM relies heavily on teamwork, often collaborating with pre-hospital providers, and demands swift, accurate decision-making to rule out deadly possibilities based primarily on presenting symptoms. |
| Ethical dilemmas | Emergency Medicine frequently presents complex ethical dilemmas. Common issues include resuscitation decisions, where physicians must make split-second 'go/no-go' choices about life support, often with incomplete information, balancing the theoretical chance of survival against meaningful benefit. Other challenges involve treating incapacitated patients (e.g., intoxicated, suicidal, or mentally ill) without explicit consent, managing violent or agitated individuals, and the fair allocation of limited resources in overcrowded EDs. Adhering to legal mandates like EMTALA, which requires treating all comers regardless of ability to pay, underscores the ethical imperative of equity. Balancing patient autonomy, beneficence, and justice, especially when honoring Do-Not-Resuscitate orders in a chaotic environment, is a continuous ethical challenge in EM practice. |
| Current trends & controversies | Emergency Medicine is a dynamic field undergoing rapid evolution. Key trends include the expansion of telemedicine into ED care, such as telestroke evaluations and remote triage, and the piloting of artificial intelligence and machine learning for diagnostic support and triage. There's a growing focus on behavioral health in the ED, addressing the rising number of patients presenting with mental illness or substance use issues due to limited outpatient options. Workforce shortages and burnout are driving innovations like virtual nursing and the increased use of advanced-practice extenders. Public health events, notably the COVID-19 pandemic, have highlighted the ED's critical role in disaster response and brought increased attention to health disparities. Future directions include enhanced pandemic preparedness, health equity initiatives, and the continued integration of new technologies like point-of-care ultrasound (POCUS) and data-driven protocols into everyday ED practice. |
Distinctive Aspects of Emergency Medicine
1. Breadth of Practice
EM doctors must be prepared for anything, seeing patients of all ages (from neonates to centenarians) and across all organ systems in a single shift. This unparalleled diversity, from treating a child's ear infection to managing adult trauma, requires a vast medical knowledge base and exceptional flexibility.
2. Time-Critical Decision-Making
The Emergency Department is a high-pressure environment where physicians often must diagnose and treat life-threatening conditions within minutes. Essential skills include quick pattern recognition and strict adherence to life-saving algorithms (e.g., airway maneuvers, stroke protocols). EM is often called the 'purest form of rapid diagnosis,' demanding swift and correct decisions to save lives.
3. Safety-Net and Social Care
The ED serves as a critical 'safety net' for vulnerable populations, including the uninsured, homeless, and mentally ill, who may lack other access to healthcare. EM physicians must recognize and address how social factors like homelessness and substance abuse significantly impact emergency care and patient outcomes.
4. Team Leadership and Communication
Emergency physicians are expected to rapidly assume leadership roles during crises like codes or mass-casualty events. They act as team captains, directing nurses, technicians, and consultants under immense stress. Strong communication, delegation, and the ability to coordinate a multidisciplinary team (including EMS and other specialties) are hallmarks of EM.
5. Ethical and High-Stakes Challenges
EM frequently involves complex ethical dilemmas, such as decisions about continuing futile resuscitations, obtaining consent from incapacitated patients, and triaging limited resources. Candidates must be prepared to discuss scenarios involving DNR orders, patient refusals, or mandatory reporting, understanding how legal mandates like EMTALA intensify the ethical landscape of EM.
Emergency Medicine Residency Interview Questions & How to Answer Them
Emergency Medicine residency interviews will test your clinical judgment, communication skills, and ability to thrive under pressure. Be prepared to discuss your approach to high-stakes scenarios, ethical dilemmas, and diverse patient populations. Here are some common questions and how to approach them:
1) How do you ensure effective communication with patients and families during emergencies?
What the interviewers are looking for: This question checks how well you can talk to patients and their families when things are really intense and scary, like in an emergency room. They want to see if you're empathetic, can stay calm, and help people feel supported even when everything's chaotic.
How to excel in your answer Start by giving clear, simple updates on what's happening and what you're doing, avoiding medical jargon. Show you understand their feelings by acknowledging their fear or stress (e.g., 'I know this is scary'). Listen actively to their concerns, even if it's just for a moment, to make them feel heard. Keep your tone calm and reassuring, and try to make eye contact or get to eye level if possible. Set realistic expectations about the fast pace of the ER and what might happen next. Check if they understood you by asking them to explain it back or if they have questions. Know when to bring in other team members (like a nurse or social worker) for extra support or to continue updates.
Mistakes to avoid: Don't just give facts and tell them to 'calm down' or 'not worry' – that often makes things worse. Avoid being cold, dismissive, or overly technical with your language. Don't ignore their emotions or expect them to simply 'trust you and let you do your job.' Don't forget to mention the unique challenges of communicating in a busy, noisy ER setting.
2) How do you approach situations where a patient refuses life-saving treatment in the Emergency Department?
What the interviewers are looking for: This question checks your ethical thinking, communication skills, and judgment in a super stressful ED situation. They want to see if you understand patient rights versus your duty to help, especially when time is short.
How to excel in your answer First, always check if the patient can actually make their own decisions (their 'capacity'). This is key! If they can't make decisions (like if they're really confused or intoxicated), your job is to act in their best interest to keep them safe. Talk to them calmly and clearly, explaining what's going on and what could happen. Really listen to why they're refusing. Get your attending involved right away, and consider bringing in other help like social workers or ethics experts. Write down everything! Document your conversations, their reasons, and who you consulted. If they have capacity and still refuse, respect their choice, but offer other ways to support them.
Mistakes to avoid: Don't just focus on saving a life without thinking about the patient's right to say no. Avoid getting frustrated or using force; stay empathetic and professional. Don't forget to assess if the patient can actually make a sound decision. Don't dismiss their reasons for refusing; try to understand them. Don't try to handle it all alone; bring in your senior doctors and other team members.
3) When several high-acuity patients arrive at once, how would you prioritize and allocate resources in the Emergency Department?
What the interviewers are looking for: This question checks if you can handle extreme pressure, make super-fast decisions, and lead your team to manage multiple life-threatening situations in a crazy busy ER.
How to excel in your answer Start by quickly assessing all patients for immediate life threats (think ABCDEs!). Explain how you'd prioritize who gets help first – usually the sickest patients with the best chance of survival. Show you can lead the team with clear, calm instructions and delegate tasks efficiently. Talk about how you'd assign limited staff, beds, or equipment where they're most urgently needed. Mention when you'd call for backup (like senior doctors or more staff) if things get too intense.
Mistakes to avoid: Don't sound panicked or like you'd freeze up under pressure. Avoid just focusing on one patient or having no real plan for the whole situation. Don't forget to mention your team, how you'd delegate, or how you'd handle limited resources.
Other residency interview questions for Emergency Medicine you should rehearse
- How do you lead and coordinate a multidisciplinary team during a resuscitation or trauma code?
- What strategies do you use to manage challenging interactions with patients or families during emergencies?
- Tell me about a time in the Emergency Department when you had to make a critical decision under pressure.
- How do you prepare to handle a diverse patient population in an ER shift, and how would you adjust your approach when switching between, say, a pediatric case and an adult trauma?
- Can you describe strategies you use to de-escalate challenging interactions, such as with an agitated patient, or when a family disagrees with your plan of care?
- If a patient in the ED demands a potentially unnecessary test or treatment, such as insisting on a CT scan for mild headache, how do you respond?
- The Emergency Department is often the safety net for patients facing homelessness, addiction, or lack of access to primary care. How would you balance immediate medical needs with these broader social challenges?
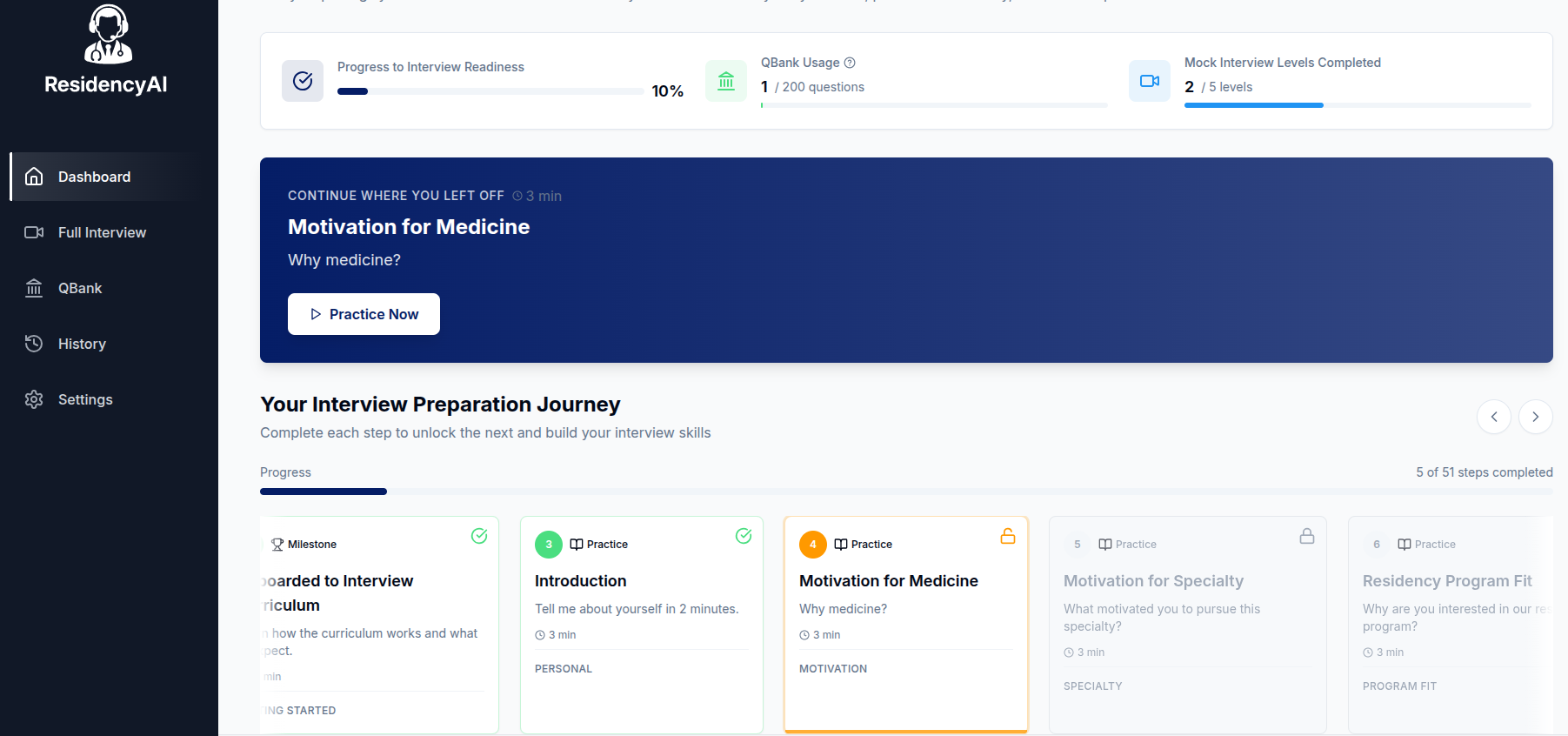
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.