General Surgery Residency Interview Questions Guide
Are you preparing for your General Surgery residency interview? This guide distills what makes General Surgery unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your General Surgery residency interview.
Table of contents
What Makes General Surgery Unique
| Patient population | General surgeons care for a very broad range of patients, including adults and often children, presenting with conditions from routine hernias to complex cancers and trauma. They serve as first-line operative care, particularly in emergencies, across diverse urban and rural communities, often providing definitive care due to surgical shortages. |
| Approaches to care | General surgeons manage a wide array of conditions, from acute abdominal emergencies (appendicitis, bowel obstruction, trauma) to elective procedures like hernia repairs, gallbladder removals, and cancer resections (colon, breast, thyroid). They utilize clinical evaluation, imaging (CT, ultrasound), and endoscopy for diagnosis. Therapeutically, they employ both open and increasingly minimally invasive (laparoscopic/robotic) techniques. They also provide perioperative critical care, including resuscitation and ICU management, coordinating multidisciplinary care for complex surgical patients. |
| Ethical dilemmas | General surgery frequently involves high-stakes, time-sensitive ethical dilemmas, such as obtaining informed consent from critically ill or incapacitated patients, balancing patient autonomy with urgent medical needs, and disclosing unexpected intraoperative findings. Other challenges include end-of-life decisions in the ICU, managing resource limitations, navigating consent for new or experimental procedures, and addressing health disparities to ensure equitable access to surgical care. |
| Current trends & controversies | General surgery is characterized by growing subspecialization and a trend towards less invasive and non-operative management for conditions like uncomplicated appendicitis or diverticulitis. Innovations include increased use of laparoscopic common bile duct explorations, robotics, and AI. The specialty also focuses on optimizing value in care and addressing workforce shortages. Demographic shifts, such as an aging and increasingly obese population, lead to more complex, high-risk patients, necessitating integration of public health measures into surgical practice. |
Distinctive Aspects of General Surgery
1. Broad Clinical Scope
General surgeons manage diseases across numerous organ systems and perform a vast array of procedures, requiring integration of knowledge from multiple fields and astute judgment on when to manage a case versus refer to a subspecialist.
2. Emergency & Trauma Readiness
A defining feature is frontline emergency and trauma care, demanding rapid assessment, decisive intervention in life-threatening situations, and the ability to stabilize patients of all ages, often under unpredictable circumstances.
3. Minimally Invasive & Advanced Techniques
The specialty has been revolutionized by laparoscopic and robotic technologies, requiring surgeons to master these advanced approaches for improved patient recovery while discerning their appropriate application versus traditional open surgery, and continuously adapting to new innovations.
General Surgery Residency Interview Questions & How to Answer Them
Preparing for your General Surgery residency interview means demonstrating not only your surgical aptitude but also your clinical judgment, ethical reasoning, and commitment to lifelong learning. Here are some common interview questions tailored to the unique demands of General Surgery, along with guidance on how to craft an exceptional response.
1) During an emergent laparotomy for suspected bowel perforation, you find extensive cancer that was not diagnosed preoperatively. How would you decide whether to proceed with resection now or stage the treatment, and how would you explain this to the patient’s family?
What the interviewers are looking for: This question presents a high-stakes, unexpected intraoperative scenario common in general surgery, designed to assess the candidate’s clinical judgment, ethical reasoning, and communication skills under pressure. Interviewers want to determine if the candidate can: 1. Prioritize immediate patient safety; 2. Demonstrate nuanced surgical oncology principles; 3. Exhibit mature ethical judgment; 4. Communicate complex, unexpected bad news effectively; 5. Involve the surgical team and other specialties.
How to excel in your answer
- Fix the immediate emergency first! Your absolute top priority is the patient's life-threatening problem (like the perforation).
- Generally, stage the cancer treatment. Explain that doing a huge cancer surgery now is too risky for an unstable patient. It's usually better to stabilize them, get a biopsy, and plan the cancer treatment properly later.
- Involve your team. Immediately consult your attending surgeon and consider getting input from surgical oncology or other specialists right there in the OR.
- Break the news gently to the family. Find a private spot, give them a 'warning shot' that you found something unexpected, and explain clearly (no jargon!) what was found and why you made the surgical decisions.
- Show empathy and outline next steps. Acknowledge their shock and grief. Explain what happens next (like pathology results, future meetings with cancer specialists, and support services like social work).
- Remember the ethical side. You're making big decisions without prior consent, so explain the 'why' to the family, focusing on what's best for the patient.
Mistakes to avoid:
- Don't try to remove all the cancer right away. That's almost always the wrong move in an emergency setting and can harm the patient more.
- Don't be blunt or dismissive with the family. This is devastating news; avoid phrases like 'they should be happy we found it.' Focus on compassion.
- Don't forget to involve your senior surgeon. You're not making this call alone, even if you're the one who found it.
- Don't just focus on the medical facts. Remember the human side – the family's emotions and future care plan are just as important.
2) You have diagnosed a symptomatic inguinal hernia that needs repair, but the patient strongly prefers to avoid surgery. How would you address their concerns and what would you consider in deciding whether to respect their wish or insist on surgery?
What the interviewers are looking for: This question assesses the candidate’s patient-centered communication skills, empathy, and ethical reasoning in a common general surgery scenario. Interviewers want to understand how the candidate balances patient autonomy with medical recommendations, especially when the patient's preference might carry significant risks. It gauges the applicant's ability to: Listen empathetically and understand the root cause of a patient's reluctance; Clearly and respectfully educate patients about diagnoses, treatment benefits, and risks of non-operative management; Navigate ethical considerations in shared decision-making; Demonstrate clinical judgment regarding the natural history and potential complications of a symptomatic inguinal hernia; Maintain professionalism and provide support.
How to excel in your answer
- Start by really listening to why the patient doesn't want surgery (e.g., fear, cost, past experiences).
- Clearly explain the benefits of surgery (pain relief, better life) and the serious risks of not having it (like needing emergency surgery later).
- Show you respect their choice, but also give your clear professional recommendation for surgery.
- Mention offering other support, like involving your attending or a social worker, and documenting everything.
- Stay calm and supportive, even if their decision isn't what you'd recommend.
Mistakes to avoid:
- Don't ignore or dismiss their concerns; try to understand them.
- Don't forget to explain the specific, serious risks of not getting surgery for a symptomatic hernia.
- Don't try to force them into surgery or sound judgmental.
- Don't forget to involve your senior doctor if the patient is refusing important care.
3) General surgeons regularly coordinate with anesthesiologists, intensivists, oncologists, and others. What do you think makes surgical leadership unique within these teams?
What the interviewers are looking for: This question aims to assess the candidate’s understanding of the unique leadership role a general surgeon plays within multidisciplinary healthcare teams. Interviewers want to know if the candidate recognizes this blend of decisive authority and the critical need for collaborative coordination with other specialists... It probes the candidate's insight into how surgical leadership differs from other medical leadership roles, emphasizing qualities like decisive action, clear communication under pressure, respect for diverse expertise, and the ability to orchestrate complex care plans from pre-op to post-op.
How to excel in your answer
- Highlight the surgeon's role as the main decision-maker, especially during the actual operation.
- Emphasize the need for clear, confident, and quick decisions, especially in emergencies.
- Show how important proactive and respectful communication is with everyone (anesthesiologists, nurses, etc.) before, during, and after surgery.
- Explain that a surgeon's leadership isn't just about giving orders, but valuing and using the expertise of all team members.
- Mention how the surgeon guides the patient's entire journey, from planning to recovery and follow-up.
Mistakes to avoid:
- Don't make it sound like the surgeon is a dictator who just tells everyone what to do.
- Avoid being vague; give specific examples of how a surgeon leads or coordinates.
- Don't forget to mention the collaborative aspect; it's all about teamwork for the patient's benefit.
Other residency interview questions for General Surgery you should rehearse
- General surgery research is advancing rapidly. How do you stay up-to-date with such developments, and how would you integrate new evidence into your practice?
- An elderly patient with late-stage pancreatic cancer requests aggressive surgical intervention. How would you weigh the potential benefits of surgery against the risks and quality-of-life considerations?
- What would you do if a patient declined a surgery you believed was the safest option for them?
- How would you approach a situation where surgery might prolong life but significantly reduce a patient’s quality of life?
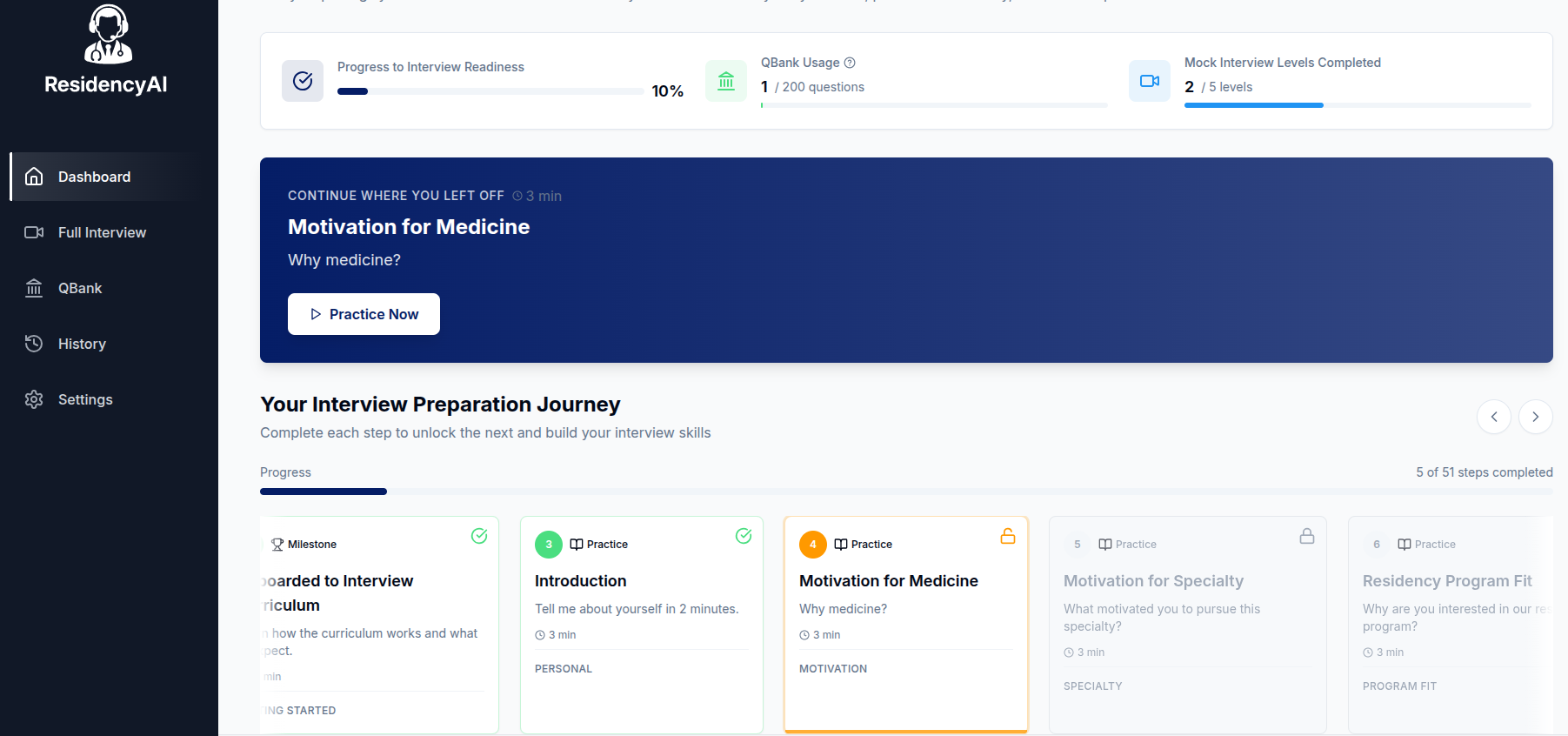
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.