Neurological Surgery Residency Interview Questions Guide
Are you preparing for your Neurological Surgery residency interview? This guide distills what makes Neurological Surgery unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Neurological Surgery residency interview.
Table of contents
What Makes Neurological Surgery Unique
| Patient population | Neurosurgeons treat patients across the entire lifespan, from neonates with congenital issues like spina bifida to adults and the elderly with acquired conditions such as brain tumors, vascular lesions, or degenerative spine disease. These patients often face life-threatening or functionally disabling conditions, meaning care decisions profoundly impact their cognition, mobility, and overall quality of life. |
| Approaches to care | Neurological surgery addresses a wide array of conditions affecting the brain, spine, and peripheral nerves, including tumors, vascular lesions, spinal disorders, trauma, CSF disorders, and functional disorders. Diagnostic approaches heavily utilize advanced imaging (MRI, CT, EEG). Treatment involves a blend of surgical techniques, from traditional open procedures to minimally invasive and endoscopic methods, alongside non-surgical management like medication and physical therapy. Modern neurosurgery also routinely incorporates stereotactic radiosurgery and endovascular treatments. |
| Ethical dilemmas | Ethical dilemmas in neurosurgery are particularly acute due to operating on the organ of consciousness. Patients and families frequently grapple with "death vs. disability" decisions, requiring neurosurgeons to balance potential benefits against risks, often involving complex considerations of patient autonomy, especially when consent is challenging. Other issues include emergency consent, disclosing surgical errors, decisions on life-sustaining measures for brain-injured patients, and managing expectations for uncertain prognoses. |
| Current trends & controversies | Neurological surgery is rapidly advancing, with a strong emphasis on minimally invasive and outpatient procedures. Technological integration is key, including intraoperative MRI, surgical robotics, and AI/machine learning for diagnostics. Research is exploring brain-computer interfaces, novel neuro-oncology drugs, and genetic therapies. Concurrently, the specialty navigates healthcare system challenges such as rising malpractice costs, evolving reimbursement models, and practice consolidation. |
Distinctive Aspects of Neurological Surgery
1. High-Stakes, Complex Anatomy
Neurosurgeons operate on the brain and spinal cord—structures vital for life, identity, and function. Even minor errors can lead to severe deficits like paralysis or cognitive loss. Candidates must demonstrate a profound understanding of risk-benefit in high-risk scenarios and a deep sensitivity to the gravity of these interventions.
2. Broad Patient/Pathology Spectrum
Neurological surgery encompasses patients of all ages, from neonates with congenital issues to elderly individuals with degenerative diseases, and covers a vast array of pathologies including trauma, cancer, and vascular lesions. Interviewers will assess your familiarity with diverse neurosurgical cases, such as the distinct considerations for pediatric versus geriatric patients, or acute emergencies versus elective procedures.
3. Technological Innovation
The specialty is a leader in adopting new technologies, including advanced microscopy, endoscopy, neuronavigation, intraoperative imaging, robotics, AI, and neuromodulation. Applicants should be prepared to discuss their commitment to staying abreast of these advancements, applying technology judiciously, and understanding the evidence base for new techniques.
4. Ethical and Communication Demands
Neurosurgeons frequently face value-laden decisions, such as choosing between aggressive surgery and comfort care. They must communicate complex and often dire prognoses to patients and families with compassion, managing expectations realistically. Interviewers will look for insight into issues like obtaining consent from incapacitated patients, making quality-of-life judgments, and transparently discussing risks.
5. Intense Training and System Pressures
Neurosurgical training is exceptionally long and rigorous, requiring immense commitment. Applicants should be aware of the demands of residency and the broader healthcare landscape, including work-life balance, burnout risks, and the evolving dynamics of private versus academic practice. Be ready to discuss how you plan to navigate these career challenges.
Neurological Surgery Residency Interview Questions & How to Answer Them
Preparing for a Neurological Surgery residency interview means being ready to tackle questions that probe your clinical knowledge, ethical reasoning, communication skills, and understanding of the specialty's unique demands. Here are some common questions you might encounter, along with guidance on how to formulate exceptional answers.
1) How would you collaborate with other specialists from oncology, neurology and critical care in the care of a complex brain tumor patient?
What the interviewers are looking for: This question assesses your understanding of multidisciplinary care, interprofessional communication, and teamwork, particularly in the high-stakes context of neurosurgery. Interviewers want to know if you recognize the distinct contributions of oncology, neurology, and critical care, and how you would proactively coordinate these inputs to optimize patient outcomes. It gauges your ability to function as part of a complex healthcare team, prioritize patient-centered care, and communicate effectively across different medical disciplines, subtly probing your leadership potential and humility.
How to excel in your answer
- Show you understand how complex brain tumors are and why many experts are needed.
- Explain what each specialist (oncology, neurology, critical care) brings to the table for this patient.
- Describe how you'd work together, like using tumor boards, daily rounds, or direct conversations.
- Always put the patient first, making sure their needs and family's wishes are central.
- Show you can lead when needed, but also respect and value everyone's expert opinion.
Mistakes to avoid:
- Don't just say you'd do the surgery and then hand the patient off. That's old-school thinking!
- Avoid making it sound like you'd just tell other specialists what to do; show you'd listen and value their input.
- Don't give super vague answers like 'we'd talk.' Be specific about how you'd communicate and coordinate.
2) How you would counsel a patient when a proposed procedure carries a significant risk of neurological deficit?
What the interviewers are looking for: This question checks if you can talk to patients and families about really serious brain or spine surgery risks with empathy, clarity, and good judgment. They want to see how you help them make tough decisions when the stakes are super high. It probes your understanding of informed consent, shared decision-making, and managing expectations when outcomes can be life-altering.
How to excel in your answer
- Set a calm, private scene and give a 'warning shot' before diving into the tough news.
- Be super clear and honest: use simple words, describe specific potential neurological problems (like 'difficulty walking' or 'memory changes'), and mention probabilities if you have them.
- Listen, listen, listen! Understand their fears and what they value most for their quality of life.
- Talk about all options, not just surgery, and make sure they feel like they're making the decision, not you.
- Offer extra support like social workers or written info, and use the 'teach-back' method to confirm they really understood everything.
Mistakes to avoid:
- Don't downplay the risks or use complicated medical jargon.
- Don't make the decision for the patient; it's their choice.
- Don't forget to ask about their values and what's important to them.
- Don't just stick to medical facts; show you care about the human side and their emotions.
3) How would principles like autonomy and quality of life influence your decision-making when treating elderly patients with severe neurological disease?
What the interviewers are looking for: This question checks your ethical compass and how you make tough decisions, especially for older patients with serious brain or spine issues. They want to see if you prioritize what the patient wants and what life means to them, not just what's medically possible. It gauges your empathy, communication skills, and ability to navigate situations where medical benefits must be weighed against personal values.
How to excel in your answer
- Start by saying these decisions are really complex and there's no easy answer.
- Always put the patient's wishes first – that's 'autonomy.' Find out what they want, or what their family says they would have wanted.
- Remember 'quality of life' means different things to different people. Ask the patient (or family) what a good life looks like for them.
- Talk clearly and kindly about all options, including risks and benefits. Listen more than you talk.
- Explain how your medical knowledge helps inform their choice, but the final decision is theirs based on their values.
Mistakes to avoid:
- Don't act like you know best and should make the decision for the patient.
- Don't just focus on keeping the patient alive without considering how they'll live.
- Avoid sounding cold or just listing medical facts without empathy.
- Don't forget to involve family or designated decision-makers if the patient can't speak for themselves.
Other residency interview questions for Neurological Surgery you should rehearse
- What factors would you consider when evaluating a patient for an experimental neuromodulation therapy?
- How would you manage unrealistic patient or family expectations of a ‘miracle cure’ after complex neurosurgery?
- How do you see emerging technologies like robotics, AI, and minimally invasive techniques shape neurosurgical care?
- How would your decision-making and communication differ in pediatric versus adult neurosurgical patients?
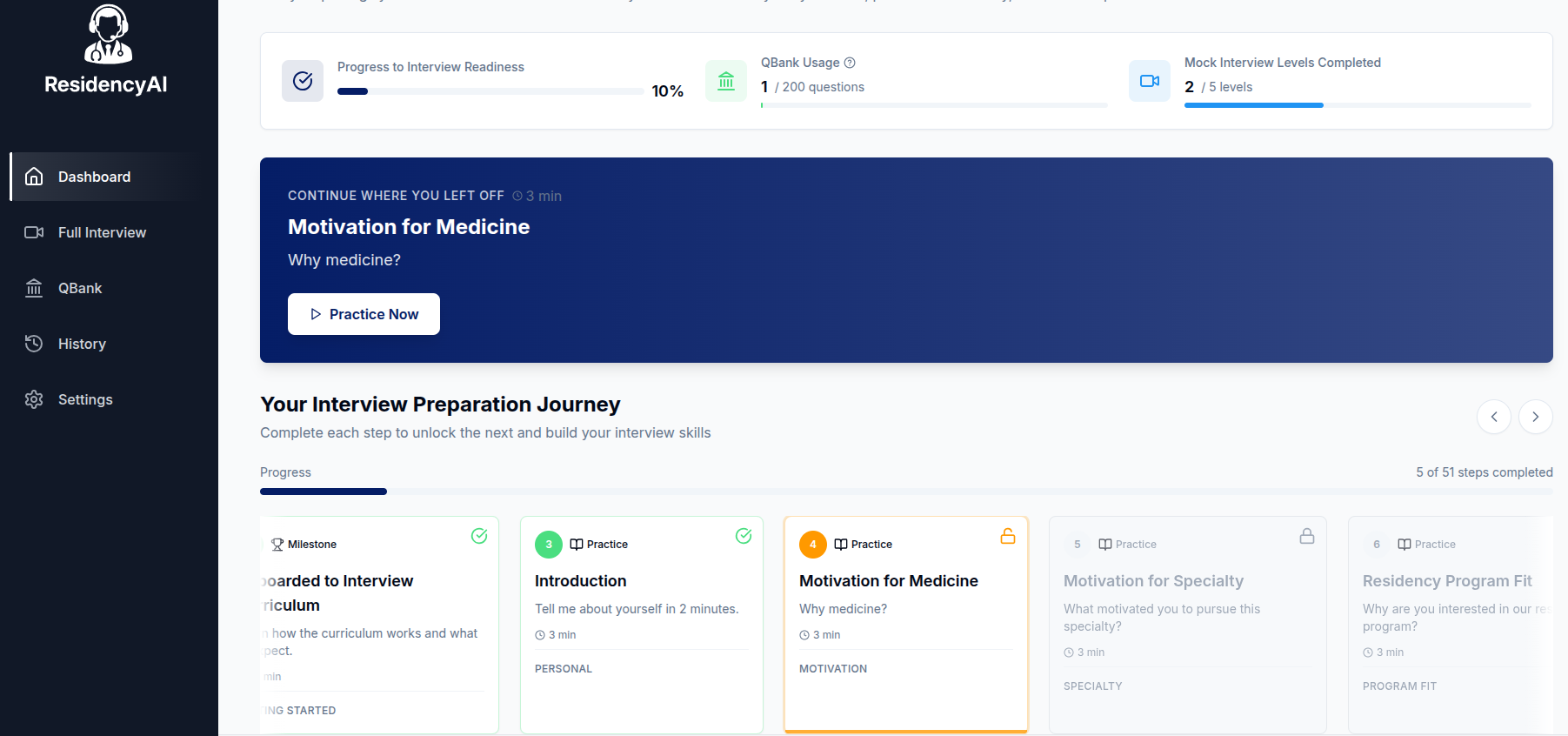
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.