Orthopaedic Surgery Residency Interview Questions Guide
Are you preparing for your Orthopaedic Surgery residency interview? This guide distills what makes Orthopaedic Surgery unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Orthopaedic Surgery residency interview.
Table of contents
What Makes Orthopaedic Surgery Unique
| Patient population | Orthopaedic surgeons treat patients of all ages -- from newborns with congenital deformities (e.g. clubfoot or scoliosis) to young athletes with ligament tears and older adults with degenerative arthritis. Common clinical problems include acute trauma (fractures, dislocations, spine or pelvic injuries), chronic degenerative conditions (osteoarthritis, osteoporosis-related fractures), sports-related injuries (meniscal tears, rotator cuff tears), spine disorders, and orthopaedic tumors. |
| Approaches to care | Diagnostic evaluation relies on physical examination and imaging (X-rays, CT, MRI). Treatment ranges from non-surgical management (rest, bracing, casts, medications or injections) to complex surgical interventions (arthroscopic repairs, open fracture fixation, joint replacements, spinal fusions). Orthopaedic surgeons often lead a multidisciplinary team, coordinating with anesthesiologists, radiologists, physical therapists, and others to optimize recovery. Extensive rehabilitation is usually required post-treatment to restore strength, motion, and function. |
| Ethical dilemmas | Key ethical issues revolve around patient-centered care and informed consent, requiring clear communication of risks, benefits, and alternatives. Balancing high patient expectations (e.g., "pain-free" joints, rapid return to sports) with realistic outcomes is crucial. Surgeons also navigate conflicts of interest (such as implant/device relationships) and ensure equitable access, avoiding bias by race, gender, or socioeconomic status. Effective communication is vital to counter the "high-tech, low-touch" perception. |
| Current trends & controversies | Technological innovation is rapidly transforming orthopaedics, with regenerative therapies (stem cells, platelet-rich plasma) and biologics explored for healing. Robotic-assisted surgery and computer navigation are increasingly used for joint replacements and spine procedures to improve accuracy. Artificial intelligence is emerging for preoperative planning and postoperative rehabilitation monitoring. Other hot topics include shifting more joint replacements to outpatient settings, debates over implant longevity, and the adoption of 3D-printed or custom implants. The specialty also addresses health disparities and workforce issues like high demand from an aging population and burnout from emergency trauma coverage. |
Distinctive Aspects of Orthopaedic Surgery
1. Broad Musculoskeletal Scope (All Ages and Activities)
Orthopaedists treat a very wide spectrum of patients -- from pediatric deformities to geriatric joint disease. Unlike many specialties, nearly anyone can present with an orthopedic issue (any age or activity level) -- from a toddler with clubfoot to an 80‑year‑old with a hip fracture.
2. Surgical/Technical Complexity
The specialty is fundamentally surgical and technical. Residents and surgeons perform many complex operations (fracture fixation, arthroscopy, joint arthroplasty, spine surgery) and must master evolving techniques. This emphasis on the operating room and hands-on procedures (often lengthy or intricate) is a hallmark. It also means orthopaedic training is rigorous and manual-skill--intensive (e.g. precise alignment in joint replacements, working around nerves and vessels in spine surgery).
3. Function and Mobility Focus with Rehab
The ultimate goal is restoring function and mobility. Orthopaedic outcomes are judged by return to movement and quality of life (walking, work, sports) rather than by treating lab values or disease remission. Thus, long-term rehabilitation and patient participation are integral -- surgeons must work with physical therapists and motivate patients through often painful recovery. Managing patient expectations about recovery timelines is uniquely important.
4. Ethical/Patient-Expectation Challenges
Orthopaedic care involves high patient expectations (many assume a surgeon can "fix" their joint or get them back to sport). Ethical dilemmas often stem from these expectations or from commercial pressures. Examples include deciding when surgery is truly indicated versus conservative management, obtaining valid informed consent for major surgeries (AAOS ethics stress explaining risks/alternatives), and disclosing any surgeon‑industry financial ties (e.g. implant royalties). Communication skills are particularly important due to the "high-tech, low-touch" stereotype and because poor communication is a leading source of grievances.
5. Innovation and Subspecialty Breadth
Orthopaedic surgery continuously adopts new technology. Issues like whether to use robot‑assisted knee replacements, how to apply regenerative PRP treatments, or how to incorporate AI-based planning are current hot topics. The field is also highly subdivided (trauma, spine, sports, pediatrics, hand, foot/ankle, oncology, etc. from adult to child), each with its controversies and cutting-edge research (e.g. best approaches to hip dysplasia in adolescents, or ethical use of imaging in spine). Staying at the forefront of these trends while critically evaluating evidence is a unique expectation of orthopaedic residents.
Orthopaedic Surgery Residency Interview Questions & How to Answer Them
Orthopaedic Surgery residency interviews delve into your clinical reasoning, ethical judgment, communication skills, and understanding of the specialty's unique demands. Here are some common questions and how to approach them:
1) How would you coordinate with physical and occupational therapists, nurses, and pain specialists to create a rehabilitation plan for a total hip replacement?
What the interviewers are looking for: This question checks if you understand that orthopaedic care is a team sport, especially for rehab. They want to see if you know how to work with different specialists to get the patient moving and feeling better after surgery.
How to excel in your answer
- Show you know what each team member (PT, OT, nurses, pain specialists) specifically brings to the rehab plan.
- Talk about clear, proactive communication methods like daily team huddles or shared notes.
- Emphasize making the plan all about the patient's goals, lifestyle, and how you'd manage their expectations.
- Mention how you, as the surgeon, would lead the team to pull all these different expert opinions together.
- Briefly touch on how you'd handle common challenges like pain management or if the patient isn't following the plan.
Mistakes to avoid:
- Don't act like you're just giving orders; show you value everyone's input.
- Avoid generic statements; give specific examples of how you'd coordinate.
- Don't forget to mention the patient's role and how you'd keep them motivated.
- Don't ignore potential difficulties in rehab; show you've thought about them.
2) Orthopaedics is seeing many technological advances such as robotic joint replacements and 3D‑printed implants. How do you stay current with these technologies, and how would you evaluate whether to adopt a new tool into your practice?
What the interviewers are looking for: This question checks if you're keen on learning, can think critically about new tech in orthopaedics, and know how to decide if a new tool is actually good for patients. They want to see you balance new ideas with what's proven and safe.
How to excel in your answer
- Mention specific ways you stay updated: reading journals, attending conferences, grand rounds, and using online medical resources.
- Explain you'd evaluate new tech based on strong evidence (like research studies) for patient safety and better outcomes.
- Talk about considering the patient's benefit, your own training needs, and the costs or ethical aspects.
- Show you're patient-focused and won't just jump on the 'latest and greatest' without good reason.
Mistakes to avoid:
- Don't say you'd only rely on what implant reps tell you or what other doctors are doing.
- Avoid sounding like you'd adopt new tech just because it's 'cool' or 'patients want it' without proof it's better.
- Don't forget to mention patient safety, research, or ethical considerations in your evaluation.
- Don't give a vague answer; be specific about your learning and evaluation process.
3) Patients often expect ‘pain-free’ results after orthopedic surgery. How would you set realistic expectations for pain and function before a procedure like a total knee replacement, especially for patients eager to resume high-impact activities?
What the interviewers are looking for: This question checks if you can talk to patients about what to really expect from surgery, especially when they have super high hopes. It shows your communication skills, empathy, and how well you understand orthopaedic outcomes.
How to excel in your answer
- Start by really listening to the patient's hopes and goals, and show you get where they're coming from.
- Explain things simply, without medical jargon. Use analogies if it helps!
- Be clear that 'pain-free' isn't always a guarantee, and some discomfort might stick around.
- Gently but firmly explain why high-impact activities are usually a no-go for new joints, and suggest safer alternatives.
- Emphasize that rehab is a huge team effort, and their commitment is key to success.
- Involve them in the discussion so they feel like a partner, not just being told what to do.
Mistakes to avoid:
- Don't dismiss their hopes or tell them they're wrong.
- Avoid promising a 'perfect' outcome or letting them think they can do anything.
- Don't use confusing medical terms without breaking them down.
- Don't forget to explain why high-impact activities are risky for the new joint.
- Don't sound impatient or like you're talking down to them.
Other residency interview questions for Orthopaedic Surgery you should rehearse
- Suppose an implant representative strongly encourages you to use a particular device or procedure. How would you respond to ensure your decision remains patient-centered and free of inappropriate influence?
- How would you incorporate a patient’s lifestyle and job requirements into your treatment plan and surgical choices?
- An active athlete with an ACL tear wants to return to play as soon as possible. How would you balance this patient’s desire for a quick recovery with evidence-based rehabilitation timelines to minimize re‑injury risk?
- For a common problem like a degenerative knee meniscus tear or early osteoarthritis, what factors would guide you to recommend surgery versus non-operative management?
- How would you approach an elderly patient who has a hip fracture but also has serious comorbidities?
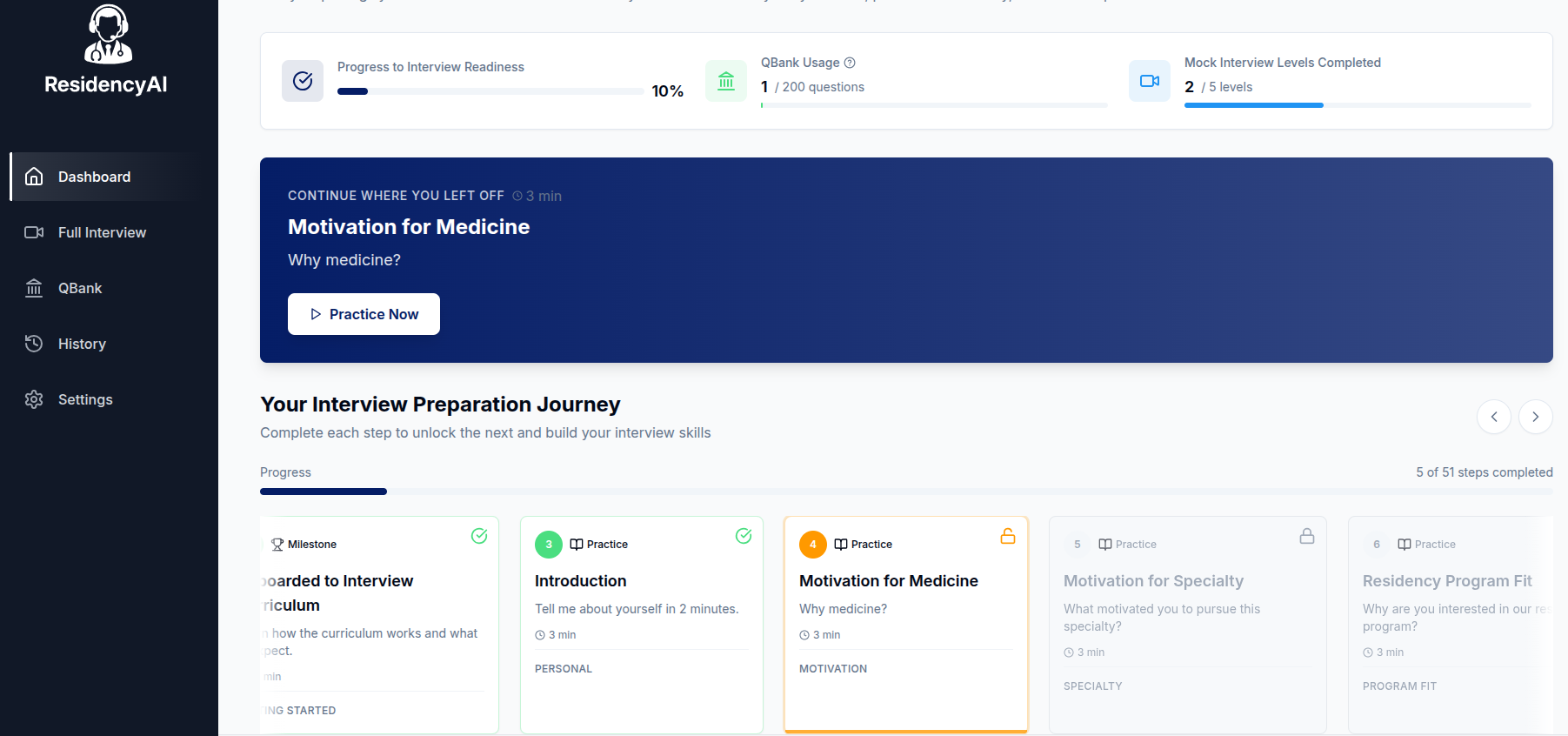
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.