Physical Medicine and Rehabilitation Residency Interview Questions Guide
Are you preparing for your Physical Medicine and Rehabilitation residency interview? This guide distills what makes Physical Medicine and Rehabilitation unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Physical Medicine and Rehabilitation residency interview.
Table of contents
What Makes Physical Medicine and Rehabilitation Unique
| Patient population | Physical Medicine and Rehabilitation (PM&R) serves a highly diverse patient population across all ages, dealing with a wide array of conditions that impair function or mobility. This includes individuals with neurological injuries (e.g., stroke, traumatic brain injury, spinal cord injury), neurodegenerative diseases (e.g., multiple sclerosis, muscular dystrophy), orthopedic and musculoskeletal problems (e.g., amputations, severe arthritis, fractures, burns), and chronic pain syndromes. The specialty also cares for children with developmental disabilities (e.g., cerebral palsy, genetic disorders, autism), athletes with sports injuries, and patients recovering from surgeries. The common thread is a functional impairment, emphasizing a 'whole person' approach to maximize independence. |
| Approaches to care | PM&R employs a multidisciplinary, goal-oriented, and patient-centered approach to care. Physiatrists lead rehabilitation teams comprising physical therapists, occupational therapists, speech therapists, social workers, and psychologists. They develop comprehensive, individualized plans to improve functional abilities, which may include prescribing exercises, adaptive equipment (e.g., wheelchairs, splints, orthotics), medications or injections for spasticity and pain, and coordinating various therapies. The specialty emphasizes long-term functional recovery, setting realistic goals with patients (e.g., walking, self-care, return to work) and measuring progress with standardized outcomes. A core principle is maximizing independence and participation in daily life, even when the underlying disease cannot be cured. Treatment settings vary from intensive inpatient rehabilitation hospitals to outpatient clinics for chronic condition management. |
| Ethical dilemmas | Ethical dilemmas in PM&R frequently center on issues of disability, fairness, and resource allocation. Challenges include determining eligibility for limited rehabilitation services (e.g., inpatient beds, therapy hours), balancing the needs of individual patients with equitable resource distribution. Other common issues involve setting realistic patient goals while balancing hope with honesty, respecting patient autonomy, especially in those with cognitive impairments, and ensuring non-discrimination in care for disabled patients. Physiatrists also navigate complexities in disability evaluation and must advocate for patients' access to assistive devices and ongoing therapy, particularly for underserved populations. |
| Current trends & controversies | Current trends and research shaping PM&R include significant advancements in technology and innovation, such as the increasing use of robotics and virtual reality to enhance therapy (e.g., robotic exoskeletons for gait training, VR games for motor rehabilitation). Tele-rehabilitation has expanded, improving access for patients in remote areas or with mobility limitations. There is a strong emphasis on evidence-based practice, utilizing functional outcome measures (e.g., gait speed, functional independence scores) and value-based care models. Subspecialties within PM&R are continuously evolving, including cancer rehabilitation, pediatric rehabilitation, women's pelvic health, sports medicine, and pain management. Controversies include optimal strategies for chronic pain management in the context of the opioid epidemic, pushing physiatrists towards multimodal pain strategies, and ensuring equitable access to rehabilitation services amidst healthcare disparities. |
Distinctive Aspects of Physical Medicine and Rehabilitation
1. Function- and Quality-of-Life Focus
The specialty centers on restoring independence in daily living and function, rather than curing disease. This goal-oriented mindset (e.g. aiming to maximize walking ability or self-care) is unique to rehab medicine.
2. Interdisciplinary Team Leadership
Physiatrists coordinate multidisciplinary rehabilitation teams (PT/OT/SLP, psychologists, social workers, etc.) to provide holistic care. Effective communication and leadership of diverse professionals is integral.
3. Broad Patient Scope
PM&R handles a wide variety of conditions and populations -- from neurological injuries (stroke, SCI, TBI) to chronic musculoskeletal problems (amputees, arthritis) and pediatric disabilities. This breadth (including sports medicine and chronic pain) requires flexibility and broad medical knowledge.
4. Chronic Rehabilitation Challenges
Many patients have chronic, non-curable conditions. Candidates must address long-term issues like spasticity, neuropathic pain, or progressive disability, requiring patience and continuity of care.
5. Ethical and Psychosocial Complexity
PM&R often involves resource allocation dilemmas, patient autonomy in face of severe disability, and cultural attitudes towards disability. Addressing disparities in rehab access and navigating complex social needs (e.g. return-to-work, family support) are essential.
6. Innovation and Research
Physiatrists adopt emerging therapies (robotics/VR) and contribute to research on functional outcomes. Trends like telemedicine, outcome measurement, and value-based care are particularly salient.
Physical Medicine and Rehabilitation Residency Interview Questions & How to Answer Them
To help you prepare, here are some common Physical Medicine and Rehabilitation residency interview questions, along with guidance on how to approach them:
1) How would you motivate and support a patient through a lengthy rehab program, especially if progress is slow?
What the interviewers are looking for: This question checks your empathy, patience, and communication skills for PM&R. They want to see how you'd keep patients motivated through tough, slow recoveries, which is super common in this field.
How to excel in your answer
- Be super empathetic: Acknowledge their frustration and validate their feelings.
- Break it down: Help them see progress by setting tiny, achievable goals and celebrating every small win.
- Involve everyone: Work with the whole rehab team (therapists, social workers, psychologists) to support them.
- Empower them: Let them be part of the plan and adapt it based on their feedback.
- Think outside the box: Mention using new tech like VR or robotics, or connecting them with support groups.
Mistakes to avoid:
- Don't blame the patient: Avoid saying it's 'up to them' or they're 'not committed enough.'
- Don't be generic: Skip vague answers like 'just be a cheerleader.' Show real strategies.
- Don't ignore the emotional side: It's not just about exercises; acknowledge their mental and social well-being.
2) Can you describe how you would incorporate psychosocial factors, such as mental health, family, into your rehabilitation plan?
What the interviewers are looking for: They want to see if you understand that rehab isn't just about fixing the body, but also about the patient's mind, family, and life situation. It shows you get PM&R's 'whole person' approach.
How to excel in your answer
- Show you understand that mental health, family, and social life are super important for recovery.
- Talk about specific ways you'd address mental health, like screening for depression or working with a psychologist.
- Explain how you'd involve the family in planning and support, maybe with a social worker's help.
- Don't forget practical stuff like housing, job goals, and hobbies – how do these fit into rehab?
- Highlight your role in leading the whole rehab team (PT, OT, social worker, etc.) to coordinate these factors.
- Emphasize empathy and tailoring the plan to each patient's unique life.
Mistakes to avoid:
- Don't just focus on physical recovery; show you care about the patient's emotional and social life too.
- Avoid saying these factors are 'soft' or just for other team members to handle – you're the leader!
- Don't just say they're 'important'; give concrete examples of how you'd incorporate them.
- Don't forget to mention how you'd lead the team to bring all these pieces together.
3) Physical Medicine and Rehabilitation is sometimes described as medicine of function. How do you define success in a patient’s rehabilitation journey when cure may not be possible?
What the interviewers are looking for: This question checks if you truly understand PM&R's focus on function and quality of life, not just curing diseases. They want to see if you can define 'success' in a meaningful way for patients with long-term conditions.
How to excel in your answer
- Shift your definition of success from 'cure' to 'maximizing function, independence, and quality of life' for the patient.
- Emphasize that success is unique to each patient, based on their personal goals and what matters most to them.
- Talk about celebrating small, consistent gains in function, showing you understand rehabilitation is often a long journey.
- Mention considering the 'whole person' – including emotional, social, and vocational factors, not just physical.
- Show you can balance realism about limitations with fostering hope and adaptation.
Mistakes to avoid:
- Don't define success as a full recovery or getting back to 'normal' – that misses the point of PM&R.
- Avoid making it about your achievements as a doctor; keep the focus on the patient's experience and goals.
- Don't give a vague answer; be specific about what functional improvements or quality of life aspects you'd prioritize.
- Don't sound dismissive or overly pessimistic about patients with chronic conditions.
Other residency interview questions for Physical Medicine and Rehabilitation you should rehearse
- How would you handle a situation where members of your rehab team disagree on a patient’s treatment plan?
- How would you counsel a patient who has high expectations for recovery but realistically has limited potential for improvement?
- How do you think rehabilitation needs differ between someone recovering from a sudden injury versus someone with a progressive condition?
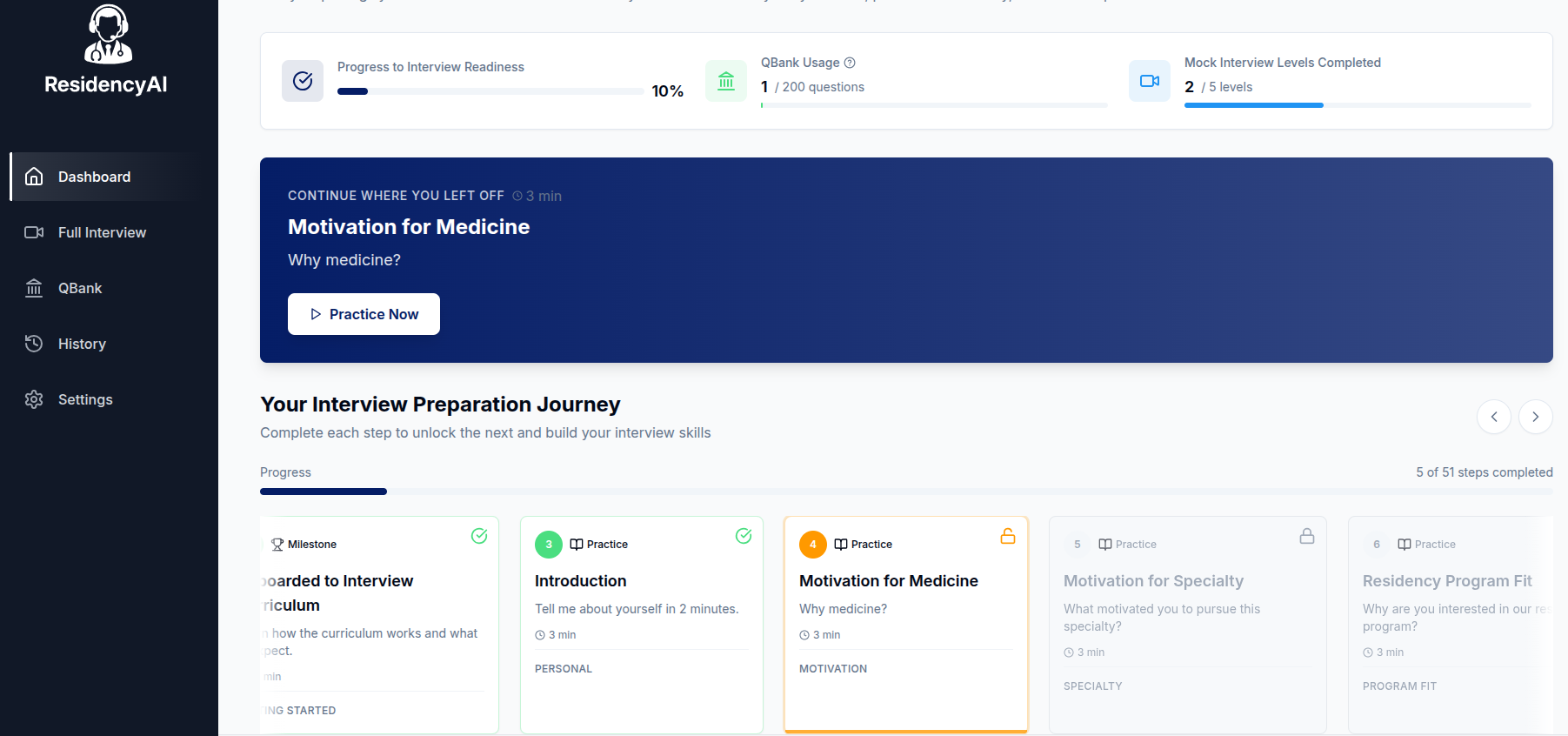
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.