Radiology Residency Interview Questions Guide
Are you preparing for your Radiology residency interview? This guide distills what makes Radiology unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Radiology residency interview.
Table of contents
What Makes Radiology Unique
| Patient population | Radiologists serve a broad patient population across all ages and specialties, as imaging is integral to nearly every field of medicine, from pediatric to geriatric patients. Unlike most clinicians, radiologists often interact more with referring physicians than directly with patients, acting as consultants who provide critical interpretations that guide diagnosis and treatment. |
| Approaches to care | Radiology encompasses a wide range of clinical problems, interpreting images of virtually every organ system to diagnose everything from fractures and appendicitis to strokes and malignancies. They frequently detect or confirm serious illnesses and manage incidental findings. The diagnostic approach is highly technology-driven, utilizing modalities like X-ray, ultrasound, CT, MRI, PET, and fluoroscopy, centering on analyzing imaging patterns and correlating them with clinical information. Radiologists also perform therapeutic interventions in Interventional Radiology (IR), offering minimally invasive, image-guided procedures. They play a key role in selecting the most appropriate imaging test and optimizing protocols. |
| Ethical dilemmas | Radiologists face unique ethical challenges, including managing incidental findings to avoid unnecessary alarm or missed diagnoses. They must weigh the benefits of imaging against radiation risks, especially in vulnerable populations. Communication ethics are crucial, involving quick relay of critical results to referring physicians and navigating direct patient communication. Error disclosure for missed findings is a significant challenge. Maintaining patient confidentiality and the obligation to report certain findings (e.g., suspected child abuse) are also key. Teleradiology introduces dilemmas regarding continuity of care, responsibility, and the balance between efficiency and community care. |
| Current trends & controversies | Radiology is rapidly evolving, with Artificial Intelligence (AI) and machine learning at the forefront, assisting in interpretation, worklist prioritization, and pathology detection, prompting discussions on AI's augmentative role. There's a push toward patient-centered radiology, encouraging more visible radiologists and improved patient communication. Multidisciplinary collaboration is increasing, integrating radiologists into teams like tumor boards. Controversies include overutilization of imaging, leading to appropriateness criteria. Teleradiology is adapting to 24/7 coverage but raises questions about local vs. outsourced roles. Subspecialization is growing, improving expert interpretation but challenging broad competency. Research explores advanced imaging techniques and theranostics. |
Distinctive Aspects of Radiology
1. Broad Consultative Role in Patient Care
Radiologists act as "doctor's doctors," consulting on cases across all specialties. They provide critical diagnostic input for virtually every type of patient and disease, despite usually having limited direct patient contact. This breadth of impact and the need to collaborate with a wide range of clinicians is a defining aspect of radiology.
2. Technology-Driven, Analytical Practice
Radiology is rooted in advanced technology and imaging science. The specialty requires strong skills in visual analysis and pattern recognition, as well as continuous adaptation to new tools (from high-resolution imaging modalities to AI software). The rapid pace of innovation in radiology is unique and shapes both training and practice.
3. Dual Diagnostic and Interventional Capabilities
Unlike most specialties, radiology combines diagnosis with therapy. Diagnostic radiologists interpret images to guide care, while interventional radiologists perform minimally invasive procedures under imaging guidance. This dual nature means radiologists can directly impact patient outcomes not only by reading scans but also by treating conditions (e.g., stopping hemorrhages, ablating tumors) without open surgery.
4. Communication & Teamwork Across Settings
Effective communication is uniquely critical in radiology -- radiologists must convey findings clearly to other physicians and sometimes directly to patients, even though they often work behind the scenes. They are integral members of multidisciplinary teams (e.g., tumor boards, emergency teams), and they face the challenge of ensuring their voice is heard to advocate for the patient despite not being the primary treating doctor. The balance between working independently in a reading room and being a collaborative team player defines the radiologist's role.
5. Ethical and Patient Safety Responsibilities
Radiologists regularly navigate ethical dilemmas specific to imaging. They must manage incidental findings appropriately, guard against unnecessary radiation exposure, obtain informed consent for contrast or procedures, and maintain high accuracy to avoid diagnostic errors. Additionally, issues like teleradiology (outsourcing reads) and limited patient interaction raise questions about responsibility, quality of care, and patient advocacy that radiologists must be prepared to address.
Radiology Residency Interview Questions & How to Answer Them
Preparing for your Radiology residency interview means demonstrating a deep understanding of the specialty's unique demands, from its technological foundation to its critical consultative role. Here are some key questions you should be ready to tackle, along with insights into what interviewers are truly seeking.
1) As a radiology resident, how would you handle a situation where attending physicians raise concerns about the quality of your reports?
What the interviewers are looking for: This question checks if you're professional, humble, and dedicated to getting better, especially with your reports. They want to see if you understand how crucial good reports are for patient care and working with other doctors.
How to excel in your answer Take the feedback seriously and own it – no excuses! Connect report quality directly to patient safety and clear communication with other doctors. Ask for specific examples of what needs improving so you can target your efforts. Outline a clear plan: review reports, study weak areas, use resources, and ask mentors for help. Show you'll follow up and keep working on it until you've improved.
Mistakes to avoid: Don't get defensive or make excuses about workload. Don't minimize the importance of your reports; they're vital for patient care. Avoid a vague plan like 'I'll just try harder' – be specific about your steps.
2) Imagine you are a radiology resident on weekend call, responsible for covering ultrasound cases while the attending is not immediately available. How would you approach this situation?
What the interviewers are looking for: This question wants to see if you can handle things on your own, make smart decisions, keep patients safe, and talk clearly, especially when your attending isn't right there. They're checking your judgment and how you'd get help if needed.
How to excel in your answer Always put patient safety and getting the right diagnosis first. Explain your step-by-step process for reading ultrasounds, like checking history and old scans. Show you're confident for easy cases but know when to ask for help on tough or critical ones. Describe how you'd quickly tell other doctors about important findings, making sure they get it. Be clear about when and how you'd call your attending – don't be shy about it for tricky cases! Mention using resources like textbooks or asking a senior resident if you're unsure.
Mistakes to avoid: Don't act like you know everything and never need your attending. Don't just wing it; show you have a plan for interpreting images. Don't hold back on telling other doctors about urgent findings. Don't hesitate to call your attending for anything complex, critical, or if you're unsure. Don't forget to mention that patient safety is your top concern.
3) what are your thoughts on the impact of AI on radiologists’ roles in the near future, and how would you adapt to work effectively with AI tools?
What the interviewers are looking for: They want to see if you're up-to-date on AI in Radiology, how you see it changing things (helping or hurting?), and if you're ready to learn and use new tech. Basically, are you forward-thinking and excited about the future of the field?
How to excel in your answer See AI as a partner that augments your role, not replaces it. It's there to make you better! Give specific examples of how AI can improve radiology (like sorting urgent cases or spotting subtle findings faster). Explain how AI will free you up to focus on what humans do best: complex thinking, consulting with other doctors, and direct patient interaction. Show you're ready to learn about AI's strengths and weaknesses, and how you'll use it smartly in your daily work. Mention how AI can lead to better patient care, more accuracy, and even less burnout for radiologists.
Mistakes to avoid: Don't dismiss AI or act like it's not a big deal for radiology's future. Don't underestimate what AI can do or resist the changes it brings to the field. Avoid saying AI is just for 'basic tasks' or that you'll only stick to human-only work. Don't sound anxious or scared about AI taking over jobs; focus on collaboration.
Other residency interview questions for Radiology you should rehearse
- What is your perspective on teleradiology?
- What are your thoughts on directly communicating imaging results to patients?
- How do you envision the radiologist’s role in patient care when you seldom meet the patient directly?
- Imagine a clinician requests a high-risk or unnecessary imaging study for a patient. How would you handle this scenario?
- If you ever realized that you missed a significant finding on an earlier study or made an incorrect interpretation, how would you handle it?
- How would you approach a situation where a referring doctor disagrees with your imaging interpretation or recommendation?
- How would you adjust your approach when performing imaging for a special population, such as children or pregnant patients?
- If you discover an incidental finding on a scan (for example, a small lesion unrelated to the scan’s purpose) that is likely benign but uncertain, how would you report and manage it?
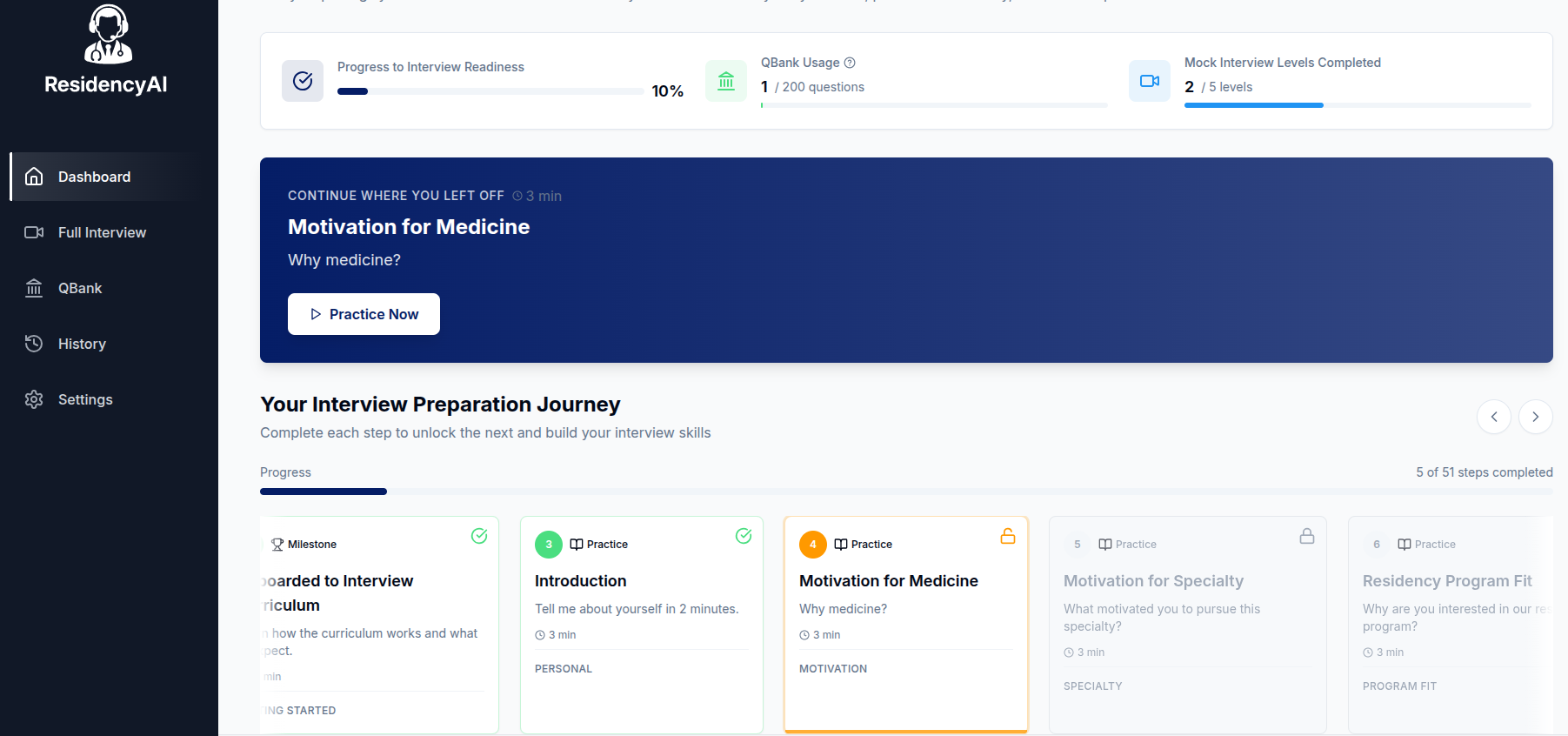
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.