Sports Medicine Residency Interview Questions Guide
Are you preparing for your Sports Medicine residency interview? This guide distills what makes Sports Medicine unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Sports Medicine residency interview.
Table of contents
What Makes Sports Medicine Unique
| Patient population | Sports Medicine physicians care for athletes and active individuals across all ages and skill levels, from professional competitors to 'weekend warriors,' youth athletes, active seniors, and non-athletes pursuing fitness. Patients are often otherwise healthy and highly motivated, seeking to optimize performance or return to activity quickly. |
| Approaches to care | The specialty addresses acute injuries (sprains, strains, fractures) and chronic/overuse injuries (tendonitis, stress fractures), as well as concussions. Care emphasizes comprehensive evaluation and conservative management, including thorough history and physical exams, imaging (X-rays, MRI, musculoskeletal ultrasound), rest, activity modification, and individualized physical rehabilitation. Medications (NSAIDs) and injections (corticosteroids, biologics like PRP) are used to facilitate healing. Collaboration with orthopedic surgeons for surgical interventions is common. A hallmark is sideline assessment and return-to-play guidance. |
| Ethical dilemmas | Sports Medicine frequently encounters ethical challenges such as the return-to-play decision, balancing an athlete's long-term health with immediate competitive goals, and managing pressure from coaches or team management. Confidentiality is a concern, especially for team doctors who may need to share injury information. Doping and performance-enhancing drugs pose significant ethical issues, requiring physicians to discourage use and counsel athletes on safe practices. Care for younger athletes raises dilemmas about advising them to limit or stop a sport for their future well-being. |
| Current trends & controversies | Key trends include evolving concussion management protocols and research into long-term risks, growing concerns about youth sports specialization leading to overuse injuries, and the rise of regenerative medicine (stem cell, PRP therapies) with ongoing scrutiny regarding evidence and safety. Technology like wearable sensors, data analytics, telemedicine, virtual reality rehabilitation, and motion analysis are transforming diagnosis and recovery. Public health initiatives like 'Exercise is Medicine' promote physical activity. Cultural issues such as playing through pain, athlete mental health, and ensuring equity for diverse athlete populations are also contemporary considerations. |
Distinctive Aspects of Sports Medicine
1. Athlete-Centered Care and Return-to-Play Focus
Sports Medicine physicians prioritize getting patients safely back to their sport or activity. This involves understanding an athlete's personal goals and the demands of their sport, and making nuanced return-to-play decisions that balance competitive timelines with medical safety. The intense focus on functional recovery and performance distinguishes sports medicine from most other fields of medicine.
2. Preventive and Performance-Oriented Approach
A unique emphasis of sports medicine is injury prevention and performance optimization, not just treatment of illness. Sports physicians proactively work on conditioning, nutrition, and biomechanics guidance to help patients avoid injury and improve athletic performance. This preventive mindset -- seeing patients before they are injured and guiding training modifications -- sets the specialty apart from general medical care.
3. Multidisciplinary Team Collaboration
Sports Medicine doctors function within a broader team of professionals (athletic trainers, physical therapists, coaches, nutritionists, sports psychologists, etc.) in the care of athletes. They must communicate effectively and often lead a coordinated care plan. The ability to collaborate and sometimes navigate differing opinions (for example, between a coach's wishes and medical advice) is a distinct aspect of the field's practice.
4. Ethical and Cultural Challenges in Sports
The specialty consistently faces unique ethical dilemmas and cultural pressures -- from decisions about clearing an athlete to play (and potential conflicts of interest as a team physician), to addressing doping, fairness, and athlete safety. Sports Medicine physicians must be prepared to handle issues like performance-enhancing drug use, confidentiality of athlete health information, managing athletes who push beyond safe limits, and advocating for patient well-being even when it conflicts with competitive goals.
5. Non-Operative Musculoskeletal Expertise and Innovation
Sports Medicine is distinct in its focus on non-surgical management of musculoskeletal injuries and its rapid adoption of new technologies/techniques. Physicians in this field develop advanced skills in musculoskeletal physical exams, imaging interpretation, ultrasound-guided procedures, and rehabilitation science -- aiming to heal injuries without surgery whenever possible. They also engage with cutting-edge treatments (like regenerative injections or novel rehab technologies) and need to critically evaluate emerging research to safely integrate innovations into care.
Sports Medicine Residency Interview Questions & How to Answer Them
Preparing for your Sports Medicine residency interview means understanding the unique challenges and rewards of this dynamic field. Here are some common questions you might encounter, along with guidance on how to provide exceptional answers.
1) Imagine you’re a team physician and a star player is pressuring to return to play before fully recovering from an injury. How would you handle this situation?
What the interviewers are looking for: This question checks if you prioritize the athlete's long-term health and safety above all else, even when facing pressure from the player or coach. It shows if you can make tough medical decisions and communicate them clearly and ethically.
How to excel in your answer
- Always put the athlete's long-term health and safety first.
- Have a private, empathetic chat with the player, explaining the risks using clear medical facts and rehab goals.
- Communicate firmly but professionally with coaches and management about medical clearance, keeping patient info confidential.
- Involve the whole sports medicine team (like athletic trainers and physical therapists) to show a united front.
- Be ready to stand by your medical decision, backing it up with evidence and protocols.
- Keep thorough notes on all your assessments and discussions.
Mistakes to avoid:
- Don't let the desire to win or please others override the athlete's health.
- Avoid suggesting quick fixes like 'masking pain' or rushing recovery against medical advice.
- Don't be wishy-washy; your medical decision needs to be firm and based on objective facts.
- Don't share private medical details with non-medical staff without the athlete's consent.
- Don't get defensive or confrontational; stay calm and professional in all your interactions.
2) Could you walk me through how you decide that a sports injury should be managed conservatively versus referring for surgical intervention? What factors influence whether you recommend rehab first or surgery right away?
What the interviewers are looking for: This question checks if you really get what Sports Medicine is all about – focusing on fixing injuries without surgery first. They want to see how you think through tough decisions, balancing an athlete's desire to play now with their long-term health.
How to excel in your answer
- Start with the injury: What kind of injury is it? How bad is it (e.g., a minor sprain vs. a full tear or broken bone)? Where is it located?
- Know your patient: Who are they? A pro athlete, a weekend warrior, a growing kid? What are their specific goals and how committed are they to rehab?
- Think about their sport: What does their sport demand? Is it a crucial part of the season or off-season?
- Explain conservative care first: Talk about rest, activity changes, physical therapy, and other non-surgical options (like injections).
- Know when surgery is needed: Explain when non-surgical options won't work or have failed (e.g., major instability, certain structural damage, or when rehab just isn't cutting it).
- Talk to everyone: Emphasize discussing options with the athlete, their family, coaches, and other team members (like physical therapists, athletic trainers, and orthopedic surgeons).
- Balance short-term and long-term: Show you care about getting them back in the game safely and for their long-term health, not just a quick fix.
Mistakes to avoid:
- Being too simplistic: Don't just say 'always try rehab first' without considering the specifics of the injury or athlete.
- Forgetting the team: Don't act like you're making the decision alone; collaboration is key in Sports Medicine.
- Ignoring the athlete's personal goals: You need to consider what the patient wants and needs, not just what's medically ideal on paper.
- Sounding rigid: Show you can adapt your plan as the injury progresses or new information comes up.
- Dismissing surgery: Don't make it sound like surgery is always a last resort or a failure; sometimes it's the best path for long-term function.
3) How do you balance an athlete’s immediate performance goals with their long-term health and well-being?
What the interviewers are looking for: This question checks if you understand the tricky balance between an athlete wanting to play now and your job to protect their future health. It shows your patient advocacy, ethical thinking, and how you handle tough conversations.
How to excel in your answer
- Always put the athlete's long-term health and safety first. Make that your top priority.
- Show empathy for their competitive drive! Acknowledge their passion and desire to get back in the game.
- Educate them clearly about risks and benefits, and involve them in making decisions about their recovery.
- Talk about a structured plan: think phased return-to-play, rehab, and bringing in the whole team (trainers, psychologists, coaches).
- Be ready to stand your ground firmly but respectfully if there's pressure to return unsafely.
Mistakes to avoid:
- Don't prioritize winning or immediate performance over the athlete's future health.
- Avoid suggesting unsafe practices like 'playing through pain' with medication.
- Don't sound dismissive of the athlete's goals; show you understand their drive.
- Don't lack a clear, proactive strategy for managing the situation.
- Don't forget to mention involving the athlete in the decision-making process.
Other residency interview questions for Sports Medicine you should rehearse
- If you were a team doctor, how would you handle media or public inquiries about an athlete’s injury and prognosis?
- Suppose you are tasked with developing an injury prevention program for a local soccer team that has had a spate of ACL injuries. How would you go about creating and implementing this program?
- As a Sports Medicine physician, you may be responsible for pre-participation physicals and clearing athletes for play. How would you handle discovering a potentially serious condition (for example, signs of a heart disorder) in an athlete who otherwise feels fine and is desperate to play?
- How would you support an athlete who is facing a potentially career-ending injury or struggling with the psychological aspects of injury recovery?
- You are evaluating a collegiate athlete who has sustained multiple concussions in one season and is eager to continue playing. How do you approach their care and counsel them about the short- and long-term risks?
- How you would approach a situation where your recommended treatment plan for an athlete differs from what the coach or trainer wants?
- If you suspected that an athlete under your care was secretly using banned performance-enhancing substances, how would you approach that situation? What balance would you strike between maintaining trust with the athlete and protecting their health, career, and the integrity of competition?
- What is your approach to pain management in injured athletes? How do you balance effective pain relief with concerns about medication side effects, dependency, or anti-doping regulations?
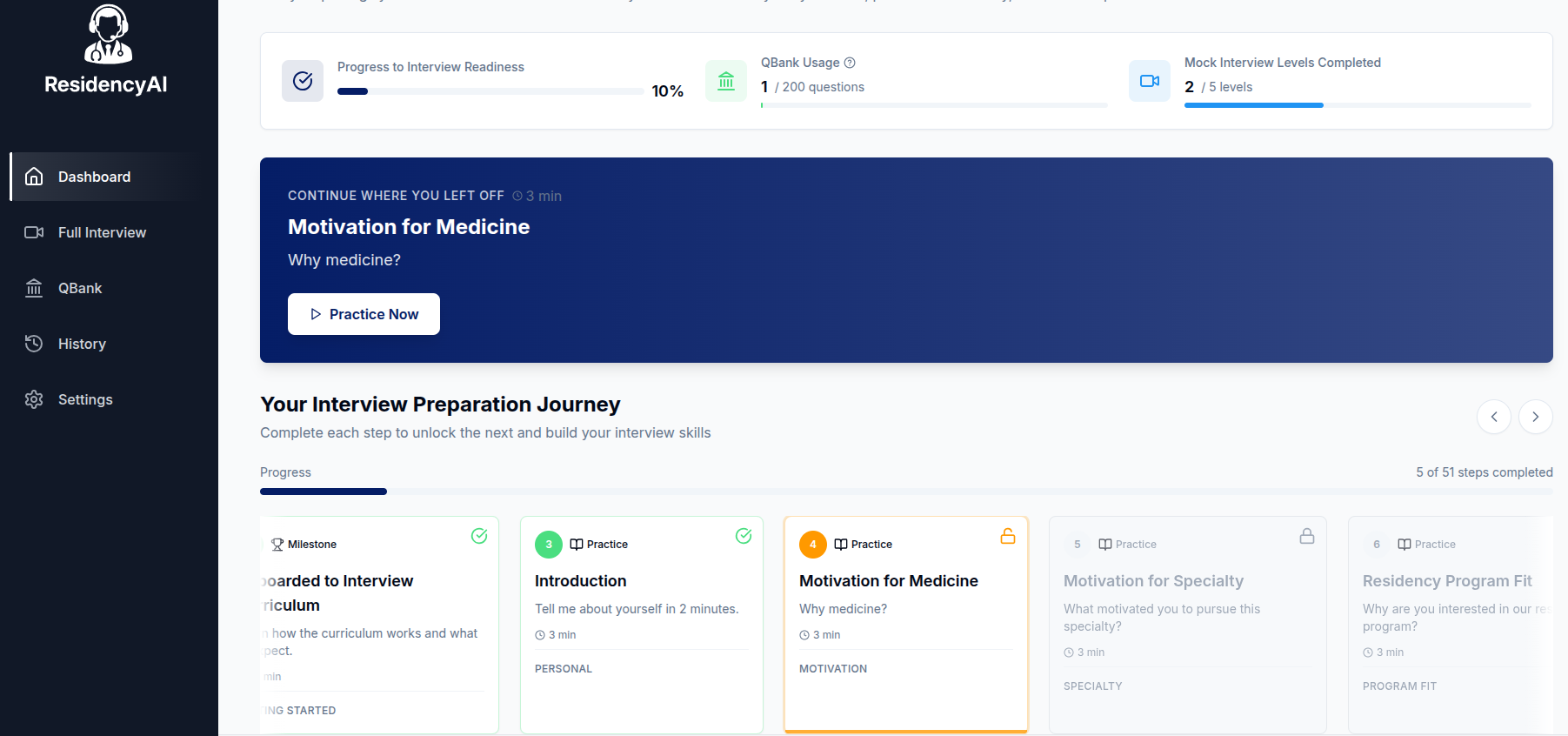
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.