Thoracic Surgery Residency Interview Questions Guide
Are you preparing for your Thoracic Surgery residency interview? This guide distills what makes Thoracic Surgery unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Thoracic Surgery residency interview.
Table of contents
What Makes Thoracic Surgery Unique
| Patient population | Thoracic surgeons treat a wide demographic, from neonates (e.g. congenital tracheal anomalies) to elderly patients. Most candidates are middle-aged or older and have smoking-related or chronic cardiopulmonary diseases. For example, lung cancer -- the deadliest cancer in the U.S. -- accounts for over 200,000 new cases per year. Many lung cancer patients also have COPD or coronary artery disease, creating a frail, comorbid population. Additionally, thoracic practice includes transplant candidates (end-stage heart or lung disease) and occasional pediatric cases (repair of tracheoesophageal fistula, correction of pectus excavatum when adults). |
| Approaches to care | Thoracic surgeons manage any operative chest pathology, including pulmonary tumors, mediastinal masses, esophageal cancer, and benign but complex issues like diaphragmatic hernias. They also address thoracic complications of non-thoracic conditions and certain vascular problems like thoracic aortic aneurysms. Specialists rely heavily on advanced imaging (CT, PET/CT, MRI, echocardiography) and functional tests (pulmonary function tests, endoscopy) for diagnosis and staging. Minimally invasive techniques (VATS and robotic surgery) are increasingly the norm for precise resections. For many cancers, surgery is integrated with chemotherapy, immunotherapy, or radiation. Thoracic teams often use intraoperative adjuncts like advanced ventilatory support or ECMO during complex airway and transplant cases. |
| Ethical dilemmas | Thoracic surgery frequently involves high-risk patients, leading to common discussions about operative futility and quality of life. Deciding whether to proceed with surgery in a very frail lung cancer patient or continuing aggressive care with a grim prognosis can be ethically complex. Transplant allocation is another key dilemma, balancing fairness with the best use of scarce donor organs. Informed consent is especially nuanced, as interventions carry significant mortality, requiring thorough explanations of risks, alternatives (including nonoperative palliative care), and advance directives. |
| Current trends & controversies | The field is rapidly evolving with expanding minimally invasive approaches like robotic-assisted thoracic surgery (RATS) and uniportal VATS for complex resections. Advances in imaging (3D CT reconstructions, virtual lung mapping) are improving surgical planning. In lung transplantation, innovations like ex-vivo lung perfusion and increased use of donation after circulatory death are prominent. Public health trends like enhanced lung cancer screening have increased detection of small lung nodules, sparking debate over management. Thoracic oncology integrates immunotherapy, raising new questions about surgical benefit. Workforce issues are also emerging, with rising demand and a looming shortage of thoracic surgeons. |
Distinctive Aspects of Thoracic Surgery
1. Comprehensive Chest Disease Management
Thoracic surgery uniquely spans multiple organ systems in the chest. Surgeons in this specialty handle diseases of the lungs, heart, esophagus, chest wall, mediastinum and diaphragm. No other specialty combines, for example, lung cancer resections with esophageal or chest wall surgeries. This broad scope requires versatility across pulmonary, cardiovascular, and oncologic domains.
2. High-Risk, High-Stakes Procedures
Thoracic surgeons routinely perform operations with significant morbidity and mortality. Typical patients are older with comorbidities (e.g. a heavy smoker with COPD undergoing lung resection). For example, even modern lobectomies carry a few-percent 30-day mortality. Ethical and clinical reasoning about risk-benefit is therefore essential. Candidates must be prepared to counsel and care for patients in critical condition (end-stage cardiopulmonary disease, massive hemoptysis, acute aortic dissection) where timing and judgment are crucial.
3. Advanced Minimally Invasive Technology
Thoracic surgery is at the forefront of surgical innovation. Video-assisted thoracoscopic surgery (VATS) is standard for many lung and esophageal cases, and robotic-assisted thoracic surgery (RATS) is increasingly used for complex resections. Surgeons plan with high-resolution 3D imaging and sometimes use intraoperative navigation. Staying current with these technologies (and their indications) is a critical aspect of the specialty's identity.
4. Thoracic Oncology and Screening
Surgical treatment of thoracic malignancies (lung cancer, esophageal cancer, thymomas, mesothelioma) is central to the specialty. Thoracic surgeons must integrate evolving oncologic therapies (chemotherapy, targeted/immunotherapy) with surgery. The rise of lung cancer screening programs has made early lung nodule management a hot topic -- deciding when to operate on small or pre-cancerous lesions (such as ground-glass nodules) is a specialty-specific challenge. Mastery of tumor board collaboration and evidence-based oncology is therefore key.
5. Ethical and Resource Allocation Challenges
Because thoracic surgery deals with scarce resources (like donor lungs) and life-threatening diseases, ethical considerations are paramount. Issues include transplant candidacy and fairness, surgical futility in terminal lung disease, and balancing aggressive intervention versus palliative care. Candidates must recognize that thoracic surgeons often navigate these dilemmas uniquely -- for example, discussing a living will before a high-risk pneumonectomy or explaining the implications of lung transplant listing.
Thoracic Surgery Residency Interview Questions & How to Answer Them
Preparing for your Thoracic Surgery residency interview means understanding the unique demands and ethical considerations of this high-stakes field. Here are some common questions you might encounter, along with guidance on how to provide exceptional answers.
1) Describe your approach to collaborating with pulmonologists, oncologists, and anesthesiologists when planning a complex esophagectomy for cancer. How do you ensure all perspectives are addressed?
What the interviewers are looking for: This question is highly specific to Thoracic Surgery, assessing the candidate’s understanding of multidisciplinary collaboration in a complex, high-stakes procedure like esophagectomy for cancer. Interviewers want to know if the candidate recognizes the critical roles of various specialists (pulmonologists, oncologists, anesthesiologists) in optimizing patient outcomes for such challenging cases. It probes the candidate's communication skills, teamwork, and ability to integrate diverse medical perspectives into a cohesive, patient-centered treatment plan. Essentially, it gauges whether the candidate can effectively lead or participate in a multidisciplinary team, ensuring all crucial viewpoints are considered to manage the patient's complex needs (e.g., respiratory function, cancer staging/treatment, and perioperative risks) before, during, and after surgery. The question also implicitly assesses the candidate's awareness of the high morbidity and mortality associated with esophagectomy and the ethical considerations involved in such aggressive interventions.
How to excel in your answer Show you know what each specialist (pulmonologist, oncologist, anesthesiologist) brings to the table for this specific surgery. Talk about structured teamwork, like multidisciplinary tumor boards or dedicated pre-op meetings. Explain how you'd make sure everyone's perspective is heard and integrated, not just that you'd 'listen'. Keep the patient at the center – connect all this teamwork back to patient safety and informed consent. Use a few specific terms or concepts from Thoracic Surgery to show your knowledge of the field.
Mistakes to avoid: Don't be vague or dismissive of any specialist's role; show you value all input. Avoid sounding like the surgeon's opinion is the only one that matters; emphasize true collaboration. Don't just say you'd 'talk to them' – explain the process of information sharing, discussion, and consensus. Don't forget to mention how this teamwork directly benefits the patient's safety and outcome.
2) How would you handle a situation where a patient with advanced lung cancer and poor functional status strongly requests surgery that you believe would be medically futile?
What the interviewers are looking for: This question checks your communication skills and ethical compass when a patient wants a surgery that won't help them. They want to see if you can be kind but honest, explore what truly matters to the patient, and guide them to the best care, even if it's not surgery.
How to excel in your answer Start by really listening to the patient and their family. Try to understand why they want the surgery and what their hopes are. Be super empathetic. Acknowledge their feelings and hopes, like 'I understand you're hoping for this surgery.' Gently but clearly explain why the surgery might not be beneficial and could even cause more harm. Use simple language, no medical jargon! Talk about other options, especially palliative care, and show how these can help them achieve their goals (like comfort, dignity, or spending time with family). Remember your ethical duty: you can't offer surgery that you truly believe is futile and harmful. You're there to do good and avoid harm. Mention bringing in other experts, like palliative care specialists or social workers, to support the patient and family.
Mistakes to avoid: Don't be blunt or dismissive. Telling them 'it won't work' without warmth or explanation is a no-go. Don't give false hope or agree to a surgery you know is futile. Don't forget to explore their true goals and values, not just what they're explicitly asking for. Don't sound cold or uncaring; empathy is key in these tough conversations. Don't abandon the patient if surgery isn't an option; show you'll continue to support their care.
3) Robotic and advanced imaging technologies are increasingly used in thoracic surgery. How do you evaluate and integrate new surgical technologies into patient care?
What the interviewers are looking for: This question checks how you think about new technology in surgery. Are you excited but also smart about using it? Do you put patients first and work with the team when bringing in new tools?
How to excel in your answer Always emphasize that patient safety and better outcomes are your top priority. Mention checking research, studies, and professional guidelines before using new tech. Explain that you'd talk to other doctors, nurses, and even hospital admin for their input. Show you understand you'd need proper training and practice to use it safely and well. Discuss how you'd talk to patients transparently about the pros, cons, and other options.
Mistakes to avoid: Don't just say you're 'excited' or that it's 'cool' without critical thought. Don't forget to mention patient safety or ethical concerns. Don't make it all about you learning new skills or boosting your resume. Don't ignore the team aspect; you can't bring in new tech alone. Don't sound like you'd use new tech on everyone, regardless of whether it's best for them.
Other residency interview questions for Thoracic Surgery you should rehearse
- Thoracic procedures are often high-risk. How would you approach obtaining informed consent from an elderly smoker with multiple comorbidities who requires a lung lobectomy for early-stage cancer?
- What role should thoracic surgeons play in broader public health issues like smoking cessation and lung cancer screening?
- How do you approach conversations with patients who face major thoracic surgery but have significant comorbidities that increase operative risk?
- When meeting a patient with advanced lung cancer, how would you balance maintaining hope with giving a realistic outlook?
- Thoracic surgeons often face requests for operations that may not meaningfully extend life. How would you respond if a family insisted on aggressive surgery despite poor prognosis?
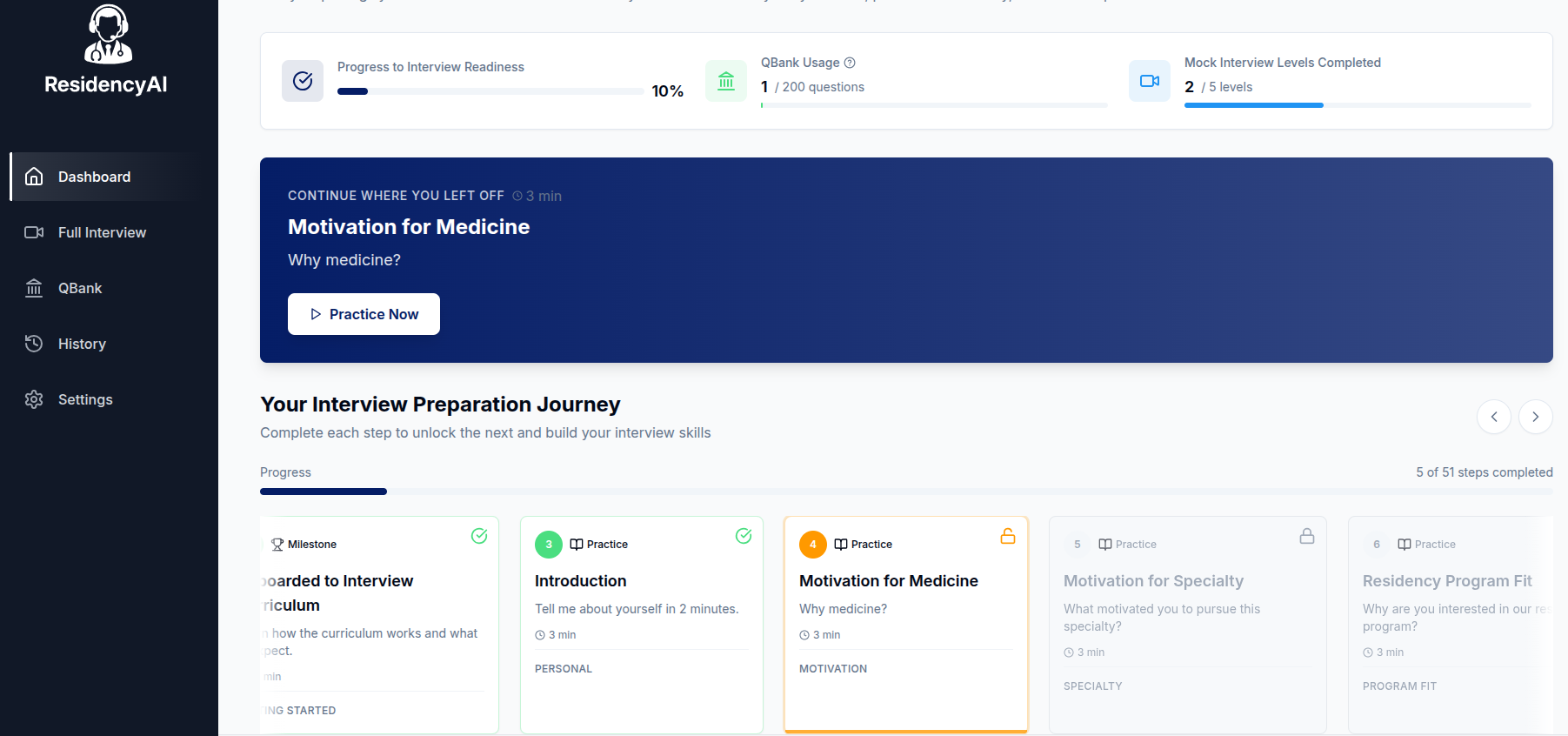
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.