Urology Residency Interview Questions Guide
Are you preparing for your Urology residency interview? This guide distills what makes Urology unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Urology residency interview.
Table of contents
What Makes Urology Unique
| Patient population | Urology is a surgical specialty focusing on disorders of the urinary tract in both men and women, as well as the male reproductive system. Urologists care for all ages, from infants with congenital urogenital anomalies to older adults with age-related conditions. While many patients are older males (e.g., due to prostate diseases), urologists also routinely treat female patients (for urinary issues like incontinence) and pediatric cases (such as congenital kidney or genital disorders). This diverse patient population requires urologists to draw knowledge from internal medicine, pediatrics, gynecology, and geriatrics. An aging population has increased the prevalence of urologic conditions, meaning urologists often serve a growing number of elderly patients with complex comorbidities. |
| Approaches to care | Urology encompasses a broad spectrum of diseases, including benign prostatic hyperplasia (BPH), urinary stone disease, urinary tract infections, bladder disorders, and urologic cancers (prostate, bladder, kidney, testicular). Urologists also manage sexual and reproductive health issues like erectile dysfunction and male infertility, as well as urinary incontinence and pelvic organ prolapse in women, and congenital abnormalities in children. The specialty is known for its technologically advanced and surgical approach, regularly performing endoscopic procedures (cystoscopy, ureteroscopy) and major surgeries, with a strong emphasis on minimally invasive techniques like laparoscopy and robotic-assisted surgery. Specialized technologies such as laser lithotripsy and shock-wave therapy (ESWL) are also utilized. While surgical, urology also involves longitudinal medical management (e.g., medications for BPH, active surveillance for low-risk cancers). Urologists frequently work in multidisciplinary teams with nephrologists, oncologists, gynecologists, and geriatricians to provide comprehensive, individualized care focused on both longevity and quality of life. |
| Ethical dilemmas | Several ethical and communication challenges frequently arise in urology due to the sensitive nature of its conditions. Prostate cancer screening (PSA testing) presents a prominent dilemma, balancing early detection benefits against risks of overdiagnosis and overtreatment. Counseling patients on aggressive treatment versus active surveillance involves principles of autonomy and non-maleficence. Managing patient expectations against evidence-based outcomes is crucial, especially for elective treatments or novel therapies. Discussions about sexual function, infertility, or incontinence demand exceptional sensitivity, respect for privacy, and cultural competence. In pediatric urology, ethical questions arise regarding genital surgery on infants with intersex conditions, with contemporary thought advocating for deferring non-urgent 'normalizing' surgeries until the patient can participate in decision-making. Ensuring informed consent and shared decision-making is critical across all aspects of urologic care, from experimental treatments to end-of-life decisions, alongside considerations for new technologies (AI, data privacy) and equitable care delivery. |
| Current trends & controversies | Urology is a dynamic field shaped by innovation and evolving best practices. Precision medicine and personalization are major trends, with new biomarkers improving prostate cancer diagnosis and reducing unnecessary interventions. Minimally invasive therapies continue to expand, including advanced endoscopic techniques and novel treatments for BPH, reducing patient morbidity. The rise of robotic surgery and AI is particularly notable, enhancing diagnostic accuracy and aiding surgical planning. Urologic oncology is seeing rapid developments in immunotherapies and new hormonal agents, requiring residents to stay abreast of clinical trials. Controversies persist in areas like optimal prostate cancer screening protocols, management of small renal masses, and the use of mesh in pelvic floor surgery. Workforce and diversity trends are also influencing the field, with a recognized shortage of urologists, increased integration of physician extenders, and ongoing efforts to improve diversity in a traditionally male-dominated specialty. |
Distinctive Aspects of Urology
1. Broad Scope & Multidisciplinary Nature
Urology spans the care of both genders and all ages, dealing with urinary and reproductive systems. Urologists must integrate knowledge from multiple fields (medicine, surgery, pediatrics, gynecology) and collaborate across specialties, making its scope uniquely broad.
2. Sensitive Patient Care & Quality-of-Life Focus
Urologic care often involves intimate issues (sexual function, continence, fertility) and non-life-threatening but quality-of-life-centric conditions. Communicating with empathy and maintaining patient dignity in these sensitive areas is a distinctive hallmark of urology practice.
3. Technological Innovation & Surgical Expertise
The specialty is defined by early adoption of new technology -- from robotic surgery to laser treatments -- and mastery of minimally invasive techniques. Urologists are expected to be at the forefront of surgical innovation and continually adapt to emerging tools that improve outcomes.
4. Complex Decision-Making & Personalized Management
Many urologic conditions have multiple management pathways (e.g. observe vs. medicate vs. operate), each with significant trade-offs. Urologists must excel in clinical reasoning and shared decision-making, tailoring treatments to individual patient risks, benefits, and preferences (e.g. choosing therapy for prostate cancer or deciding on intervention for kidney stones).
5. Ethical Challenges & Evolving Controversies
Urology faces unique ethical and societal issues -- from debates over screening and overtreatment (especially in prostate cancer) to decisions about irreversible interventions in vulnerable populations (like pediatric DSD cases). Additionally, current trends (AI in healthcare, workforce shortages, diversity efforts) pose questions about how the field should evolve. A strong urology candidate recognizes these controversies and can discuss approaches to navigating them responsibly.
Urology Residency Interview Questions & How to Answer Them
To help you prepare, here are some common Urology residency interview questions, along with guidance on how to approach them effectively.
1) Can you describe your approach to building patient trust and ensuring comfort when dealing with an intimately personal urologic issue?
What the interviewers are looking for: This question checks your empathy and communication skills, especially when talking about sensitive urologic topics like sexual health or incontinence. They want to see if you can make patients feel comfortable and build trust with them.
How to excel in your answer Show you understand how sensitive and personal these topics can be for patients. Describe how you create a safe, private, and non-judgemental space for the patient to talk. Emphasize active listening and speaking clearly, without medical jargon. Mention asking for explicit permission before discussing sensitive topics or performing physical exams. Always offer a chaperone for physical examinations, as a standard practice for patient comfort.
Mistakes to avoid: Don't be dismissive of the patient's potential embarrassment or discomfort. Avoid rushing the conversation or using overly clinical language. Don't forget to offer a chaperone for physical exams; it's a key part of ensuring comfort. Don't assume patients should 'just get over it' or won't be embarrassed.
2) How would you counsel a 55-year-old man who requests a PSA test, balancing his concerns about cancer with the risks of overdiagnosis and overtreatment?
What the interviewers are looking for: This question checks if you can handle tricky conversations about medical tests, especially when there are pros and cons. They want to see if you understand the PSA test's complexities, can explain them clearly, and help patients make their own choices.
How to excel in your answer Start by showing empathy for the patient's worries about cancer. Clearly explain both the potential benefits (like catching aggressive cancer early) and the significant risks of PSA screening. For risks, specifically mention 'overdiagnosis' (finding harmless cancers) and 'overtreatment' (unnecessary procedures with side effects like incontinence or erectile dysfunction). Stress that it's their decision. Ask about their personal priorities and what matters most to them. Keep your tone calm, informative, and unbiased – don't push your own opinion. Offer ongoing support, no matter what they decide.
Mistakes to avoid: Don't just agree to order the test without a full discussion of pros and cons. Avoid only talking about the good parts or only the bad parts; be balanced. Don't sound like you're telling them what to do, or dismiss their concerns. Don't skip explaining why it's controversial (overdiagnosis/overtreatment).
3) Can you give an example of a urologic condition that requires a multidisciplinary approach and how you would coordinate care as a urologist?
What the interviewers are looking for: This question checks if you understand that urology isn't a solo act! They want to see if you know when to team up with other specialists and how you'd actually make that teamwork happen for the best patient care.
How to excel in your answer Pick a urologic condition that clearly needs a team of different doctors (like bladder cancer or complex kidney stones). Name the specific types of specialists you'd work with (e.g., oncologists, nephrologists, pathologists, social workers). Explain how you, as the urologist, would coordinate their care. Think about tumor boards, clear communication, and involving the patient. Briefly explain why each specialist is important for that specific condition. Show how this teamwork leads to better outcomes and quality of life for the patient. Be specific! Give examples of actual coordination steps you'd take.
Mistakes to avoid: Don't pick a simple condition that doesn't really need a big team. Avoid just saying you'd 'refer' the patient. Explain how you'd actively collaborate. Don't be vague about your coordination plan; show you've thought about the practical steps. Forgetting to mention the patient's role in decision-making or their overall well-being.
Other residency interview questions for Urology you should rehearse
- Urologists manage everything from a child with a congenital anomaly to an older adult with prostate cancer. How would you adapt your approach to care for such diverse patients?
- How do you see yourself balancing enthusiasm for new tools like robotic surgery or AI-assisted diagnostics with the responsibility to ensure safety, evidence-based outcomes, and patient-centered care?
- A patient with low-risk prostate cancer is weighing surgery, radiation, or active surveillance. How would you approach counseling him through this decision?
- In pediatric urology, parents may request elective surgery for a child with an intersex condition. How would you navigate this, balancing parental wishes, patient autonomy, and current guidelines?
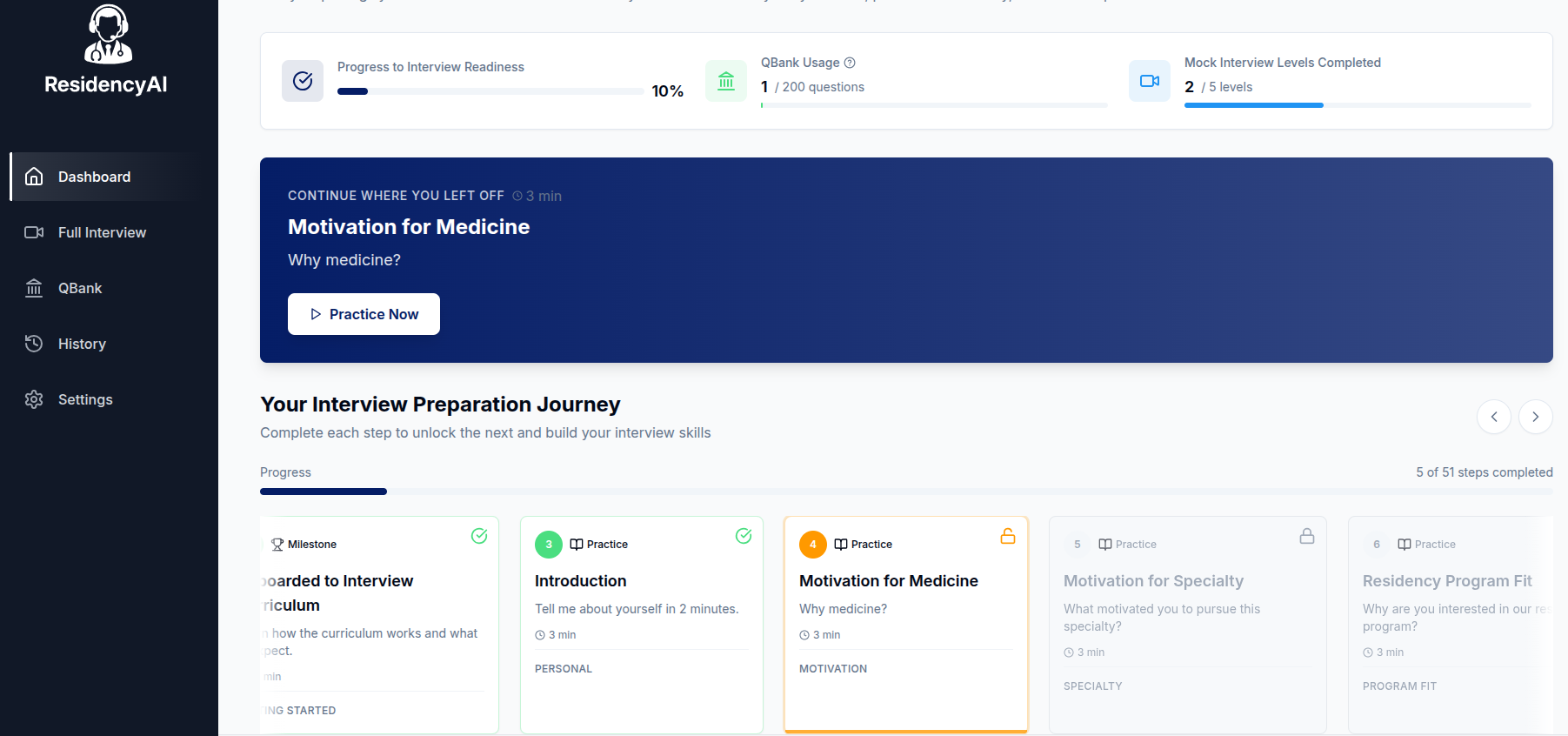
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.