Vascular Surgery Residency Interview Questions Guide
Are you preparing for your Vascular Surgery residency interview? This guide distills what makes Vascular Surgery unique and equips you with clear frameworks, sample responses, and pitfalls to avoid so you can shine on any specialty-specific questions that come your way during your Vascular Surgery residency interview.
Table of contents
What Makes Vascular Surgery Unique
| Patient population | Vascular surgeons primarily care for older adults with atherosclerotic risk factors (smoking, diabetes, hypertension, dyslipidemia). Millions of Americans have peripheral arterial disease (PAD) and abdominal aortic aneurysms (AAA); African Americans and patients over 50 are especially vulnerable to PAD. Because many patients are elderly or have chronic conditions (e.g. diabetes), the vascular surgery patient population is medically complex and often requires long-term follow-up. |
| Approaches to care | Vascular surgeons manage the full spectrum of blood-vessel disorders (arterial, venous, lymphatic) except the heart and intracranial vessels. Typical conditions include atherosclerotic PAD (leading to claudication or critical limb ischemia), aneurysms (aortic, iliac, popliteal, etc.), carotid artery stenosis (stroke prevention), mesenteric ischemia, dialysis access creation, venous insufficiency (varicose veins, deep vein thrombosis), and peripheral vascular trauma. Vascular surgeons also treat lymphatic problems (e.g. lymphedema) and neurovascular compression syndromes. Many patients present with non-healing wounds or gangrene requiring limb-salvage decisions. Vascular surgery uniquely combines noninvasive diagnostics (e.g. arterial duplex ultrasound, CT/MR angiography, plethysmography) with advanced interventions. Treatment options range from medical and endovascular (angioplasty, stenting, EVAR/TEVAR, catheter-based thrombolysis) to open surgical techniques (bypass grafts, endarterectomy, aneurysm repair). Vascular surgeons are trained in all modalities: they use evidence-based medical therapy (antiplatelets, statins, risk-factor control) alongside minimally invasive and open procedures to achieve the best patient outcome. Because vascular diseases are often chronic and progressive, longitudinal management (e.g. graft surveillance, wound care, risk-factor modification) is a hallmark of the specialty. |
| Ethical dilemmas | Common ethical challenges in vascular surgery revolve around high-risk interventions and limb salvage. For example, deciding whether to attempt complex limb revascularization or proceed with amputation involves weighing beneficence versus non-maleficence and respecting patient autonomy. Surgeons frequently care for frail, elderly patients (e.g. advanced AAA or critical limb ischemia) where the risk of surgery is high; balancing quality of life, patient wishes, and surgical futility is a recurring dilemma. Other ethical issues include allocating limited resources (urgent OR time, specialized care) and addressing disparities in access. Studies note disparities in limb-salvage rates based on geography and socioeconomic status. Vascular surgeons must often lead shared decision-making discussions, presenting best- and worst-case scenarios to patients facing life-changing procedures. |
| Current trends & controversies | Vascular surgery is rapidly evolving. Endovascular technologies continue to expand indications (e.g. fenestrated stent grafts for complex aneurysms) even as open surgery remains essential. Recent major trials are reshaping practice: the BEST-CLI trial (2023) showed that, in patients with critical limb ischemia and good vein conduit, bypass surgery had lower rates of limb loss or death than endovascular therapy. Device safety is also a trend: a 2018 meta-analysis raised concerns about paclitaxel-coated balloons/stents, but updated analyses and FDA review in 2023 found no excess mortality risk. Screening guidelines (e.g. for AAA) and gender differences are debated; for instance, current data do not support routine AAA screening in women absent other risk factors. Workforce and practice trends (training integrated vs. traditional, scope of practice with interventional radiologists/cardiologists) are also active topics in the field. |
Distinctive Aspects of Vascular Surgery
1. Comprehensive Vascular Scope
Vascular surgeons treat the entire arterial, venous, and lymphatic systems of the body (excluding the heart and brain vessels). This breadth requires understanding of diverse pathologies from carotid artery disease to deep venous thrombosis.
2. Dual Skill Set -- Endovascular and Open Surgery
The specialty uniquely demands proficiency in both minimally invasive endovascular techniques and traditional open surgery. A modern vascular surgeon chooses the optimal modality (e.g. angioplasty vs. bypass) based on patient factors and anatomy.
3. Management of High-Risk, Chronic Patients
Vascular patients often have multiple comorbidities (diabetes, smoking, renal failure) and require long-term follow-up. The specialty emphasizes aggressive risk-factor control (medical therapy, lifestyle changes) alongside procedural care. Continuity of care (wound management, graft surveillance) is a core aspect.
4. Ethical Complexity and Patient-Centered Decisions
Vascular surgery frequently involves life-altering choices (e.g. limb salvage vs. amputation, or high-risk aneurysm repair) that engage ethical principles like autonomy, beneficence, and justice. Candidates must be prepared to discuss how they would counsel patients about risks and realistic outcomes.
5. Rapidly Evolving Field with Technology and Research
Innovations (new endografts, imaging, interventions) and high-impact trials (e.g. BEST-CLI for CLI, EVAR long-term outcomes) continuously shape practice. Controversies (device safety, screening guidelines) and multidisciplinary interactions (with IR, cardiology, nephrology) are central, requiring up-to-date knowledge and teamwork.
Vascular Surgery Residency Interview Questions & How to Answer Them
Preparing for your Vascular Surgery residency interview means understanding not just the technical aspects of the field, but also its unique patient population, ethical challenges, and the collaborative nature of care. Here are some key questions you should be ready to answer, along with insights into what interviewers are truly looking for.
1) What ethical considerations would you take into account when evaluating a very elderly, frail patient for a vascular procedure like an aortic aneurysm repair?
What the interviewers are looking for: This question wants to see if you understand the tough ethical choices when operating on very old or frail patients. It's about balancing helping them (fixing the problem) with not harming them (risks of surgery) and respecting what they want.
How to excel in your answer
- Show you get it: Acknowledge that elderly, frail patients have higher risks and a tougher recovery.
- Talk about the 'Big 4' ethics: Mention patient's choice (autonomy), doing good (beneficence), avoiding harm (non-maleficence), and their quality of life.
- Explain how you'd talk to them: Describe how you'd clearly explain risks/benefits, ask about their goals and what a good life means to them, and discuss realistic outcomes (best to worst case).
- Team up: Mention bringing in other experts like geriatricians or palliative care to get a full picture.
Mistakes to avoid:
- Don't just focus on 'can we fix it?': Don't only talk about if they're medically cleared for surgery.
- Avoid being a 'boss': Don't sound like you're telling them what to do; it's their decision.
- Don't brush off age/frailty: Saying 'age is just a number' can sound dismissive.
- Forget their life: Don't forget to talk about how the surgery might affect their quality of life or what they value.
2) Vascular cases often involve interventional radiologists, cardiologists, and others. Can you give an example of how you would coordinate care and make decisions in a complex case involving multiple specialists?
What the interviewers are looking for: Vascular surgery means teaming up with lots of different doctors. This question checks if you understand how crucial that teamwork is, and if you can lead and make smart choices when many experts are involved, always keeping the patient's best interest at heart.
How to excel in your answer
- Share a specific, complex vascular patient case where multiple specialists were definitely needed (e.g., a patient with a bad leg infection AND heart problems).
- Explain how you'd get everyone on the same page. Think about team meetings, sharing all the patient's info, and directly talking to each specialist.
- Show you respect everyone's expertise and value what each specialist brings, even if their ideas are different.
- Make it clear that the patient's wishes and overall well-being are the main goal when making decisions.
- Mention using the latest research or guidelines to help make the best choice, and that you'd involve a senior vascular surgeon if there's a big disagreement.
Mistakes to avoid:
- Don't act like your specialty is the only one that matters or that you'd just tell other doctors what to do.
- Avoid being vague; just saying 'I'd coordinate' isn't enough – give specific actions you'd take.
- Don't forget to include the patient's voice and preferences in the decision-making process.
- Avoid sounding confrontational or dismissive of other specialties' opinions.
3) How do you balance patient expectations with realistic outcomes when counseling for elective vascular procedures, such as cosmetic vein treatments or repair of a small aneurysm?
What the interviewers are looking for: This question checks your bedside manner, empathy, and how well you communicate tricky information. They want to see if you can explain medical realities clearly while still respecting what a patient hopes for, especially when it comes to elective procedures.
How to excel in your answer
- Start by actively listening to what the patient expects or hopes to achieve from the procedure.
- Explain the benefits, risks, limitations, and alternatives clearly and simply, avoiding medical jargon.
- For cosmetic treatments, emphasize 'improvement' rather than 'perfection' and mention potential for recurrence.
- For more serious procedures like aneurysms, discuss all options (even watchful waiting) and the long-term commitment needed.
- Involve the patient in the decision-making process; it's about their informed choice.
- Stay calm, patient, and empathetic, even if their expectations are far from reality.
Mistakes to avoid:
- Don't just rattle off facts; ignore the patient's feelings or hopes.
- Avoid making promises you can't guarantee, especially for cosmetic results.
- Don't dismiss a patient's expectations as 'unrealistic' in a blunt or condescending way.
- Don't make the decision for the patient; empower them to choose.
- Don't use too much technical medical language without breaking it down.
Other residency interview questions for Vascular Surgery you should rehearse
- How do you see the identity of a vascular surgeon as distinct from other specialists, like interventional cardiology or radiology, who also perform procedures on blood vessels?
- Vascular patients often require long-term relationships with their surgeons. How would you approach building trust with a patient who will likely need ongoing follow-up for life?
- What would you do if a patient wanted a high-risk vascular operation that you believed had little chance of improving their quality of life?
- Vascular surgery often involves life-or-limb decisions. How do you think you would handle the emotional weight of counseling patients and families in these circumstances?
- Imagine a patient refuses a recommended vascular procedure despite clear risks of disability or death. How would you balance respecting autonomy with your duty to protect them?
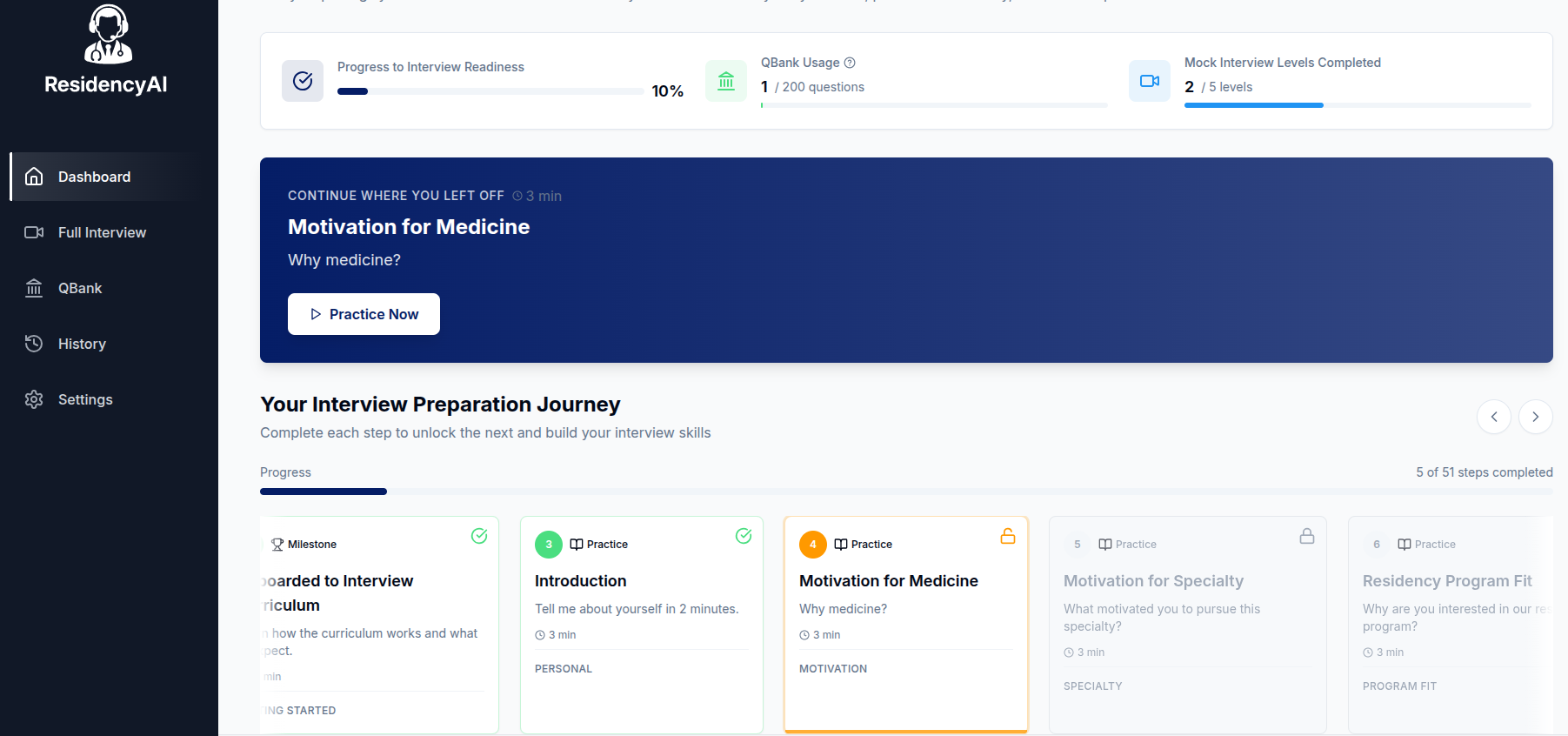
Ready to practice your interview skills?
Try AI-powered mock interviews and get instant, actionable feedback.